If you’re thinking “why is my pussy hot?” or you feel a burning vagina sensation, you’re not alone. Genital heat or burning can range from totally normal (increased blood flow when you’re turned on) to a red-flag symptom that needs medical attention. The tricky part is that vaginal burning isn’t one condition—it’s a symptom with many potential causes: friction from sex toys or tight leggings, skin irritation from soaps or laundry pods, yeast or bacterial infections, urinary tract issues, hormonal dryness, recently shaved/waxed skin, and more. Sometimes there’s no discharge but burning sensation; other times you’ll notice itching, odor, or changes in urination.
This guide breaks everything down simply: common causes, quick self-care that’s actually safe, what to avoid, and when to see a clinician. We’ll also cover prevention (lube, breathable fabrics, toy hygiene) and answer the most-asked questions in plain language. If symptoms are severe, you’re pregnant, or you feel unwell, skip the home fixes and get checked—otherwise, use this as a calm, practical roadmap back to comfort.

Normal heat vs. problematic burning
A warm, flushed feeling during arousal is normal: blood vessels dilate, tissues swell slightly, and the vulva can feel hotter or pulsing. That should not sting, itch, or burn after touch stops.
Burning or “hot” that suggests a problem tends to be:
- Persistent (lingers after sex/workouts)
- Stinging with pee, wiping, or penetration
- Accompanied by itching, odor, unusual discharge, sores, swelling, spotting, or fever
- Triggered by products (new body wash, scented wipes, new detergent, new lube/condoms)
If that sounds like your situation, skim the causes below and go straight to the relief and when to see a doctor sections.
Friction, clothing, and grooming (the under-rated culprits)
- Dry sex or long sessions without enough lube → microtears and burning after.
- Tight synthetic leggings/underwear, especially when damp after workouts → heat rash, chafing, folliculitis.
- New razor/wax → razor burn, ingrown hairs, raw skin that stings with soap/urine.
- Post-swim sit-arounds → wet suits trap heat and bacteria on delicate skin.
What helps now: cool compress (clean, damp cloth) for 5–10 minutes, switch to loose cotton underwear, avoid friction for 24–48 hours, and use plenty of water-based lube next time. If grooming, use fresh blades, shave with slip (conditioner/lube), and rinse with lukewarm water—no perfumes on freshly shaved skin.
Irritant or allergic contact dermatitis (soaps, wipes, lubes, latex)
- Scented soaps, bubble bath, bath bombs, wipes, scented period products
- Laundry pods/fabric softeners left in underwear
- New lube ingredients (menthol/tingle, warming agents, flavors, dyes), glycerin if you’re yeast-prone
- Condom materials: latex allergy or intolerance to certain lubricants/spermicides on condoms
- Deodorant sprays, talc, vaginal douches (skip these entirely)
What helps now: rinse gently with lukewarm water only (no internal douching), switch to unscented, pH-gentle products, and avoid the suspected trigger for at least a week. If condoms are the issue, try non-latex options and a simple water-based or aloe-based lube with a short ingredient list.

Infections: yeast, BV, UTIs, and some STIs
Yeast (vulvovaginal candidiasis)
Burning + itching, thick/white discharge, redness. Can follow antibiotics, tight/sweaty clothes, high sugar, or new products. Self-treating with OTC antifungals only makes sense if you’ve had a clinically diagnosed yeast infection before and symptoms match; otherwise, test first—BV/STIs can look similar.
BV (bacterial vaginosis)
Burning/irritation with thin, gray/white discharge and fishy odor, often after sex or menses. Needs prescription treatment; probiotics and home remedies won’t reliably fix BV.
UTI (urinary tract infection)
Burning with urination, urgency, frequent small pees, sometimes lower-abdomen pressure; vaginal discharge is usually not the main feature. A urine test confirms it.
STIs (e.g., chlamydia, gonorrhea, trichomoniasis, herpes)
Can cause burning, pain, discharge, spotting, or sores—sometimes no symptoms. Testing is the only way to be sure.
Bottom line: If you have burning plus discharge/odor/fever/sores, or symptoms persist >48–72 hours, get medical evaluation instead of guessing.
Hormones, skin conditions, and “burning with no discharge”
- Low estrogen (perimenopause/menopause, postpartum, some birth control): thins and dries vaginal tissue → burning with sex/peeing. Vaginal moisturizers, lubricants, and clinician-guided local estrogen can help.
- Vulvodynia/vestibulodynia: nerve-based burning at the entrance (vestibule), often worse with touch; needs specialized care (pelvic-floor PT, topical treatments, desensitization).
- Lichen sclerosus, eczema, psoriasis: inflammatory skin issues cause burning, tearing; exam + prescription therapy are key.
- Pelvic-floor hypertonicity (vaginismus): muscles guard/tighten, causing burning with penetration; pelvic-floor physical therapy works wonders.
Relief that actually helps (and what to avoid)
Do this (gentle, evidence-friendly):
- Cool compress 5–10 minutes, 2–3×/day day one; lukewarm sitz bath (plain water) if soothing.
- Loose, breathable underwear; change damp clothes fast.
- Water-based lube during any sexual activity; avoid penetration until stinging resolves.
- OTC pain relief (e.g., ibuprofen/acetaminophen) if you can take them safely.
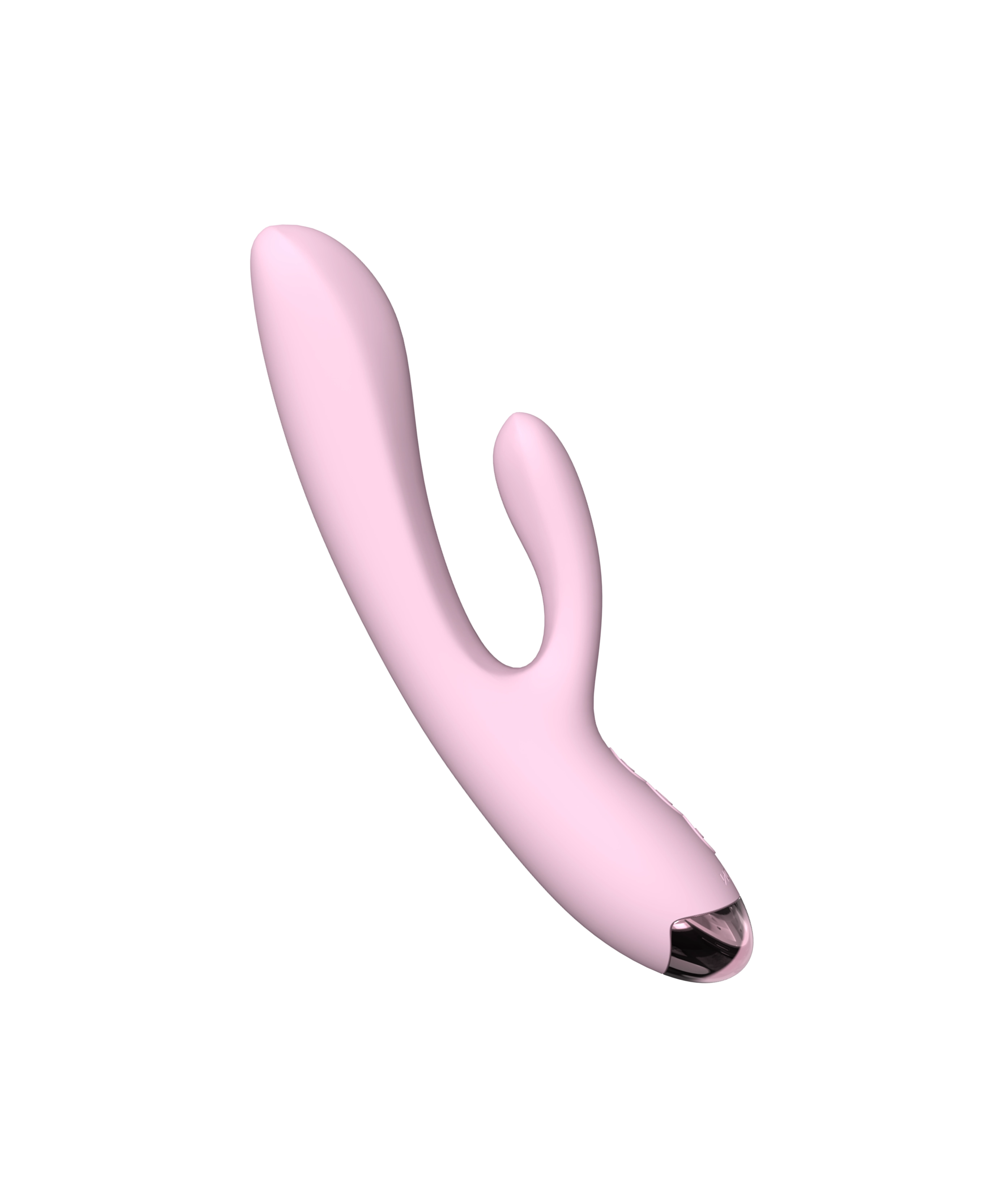
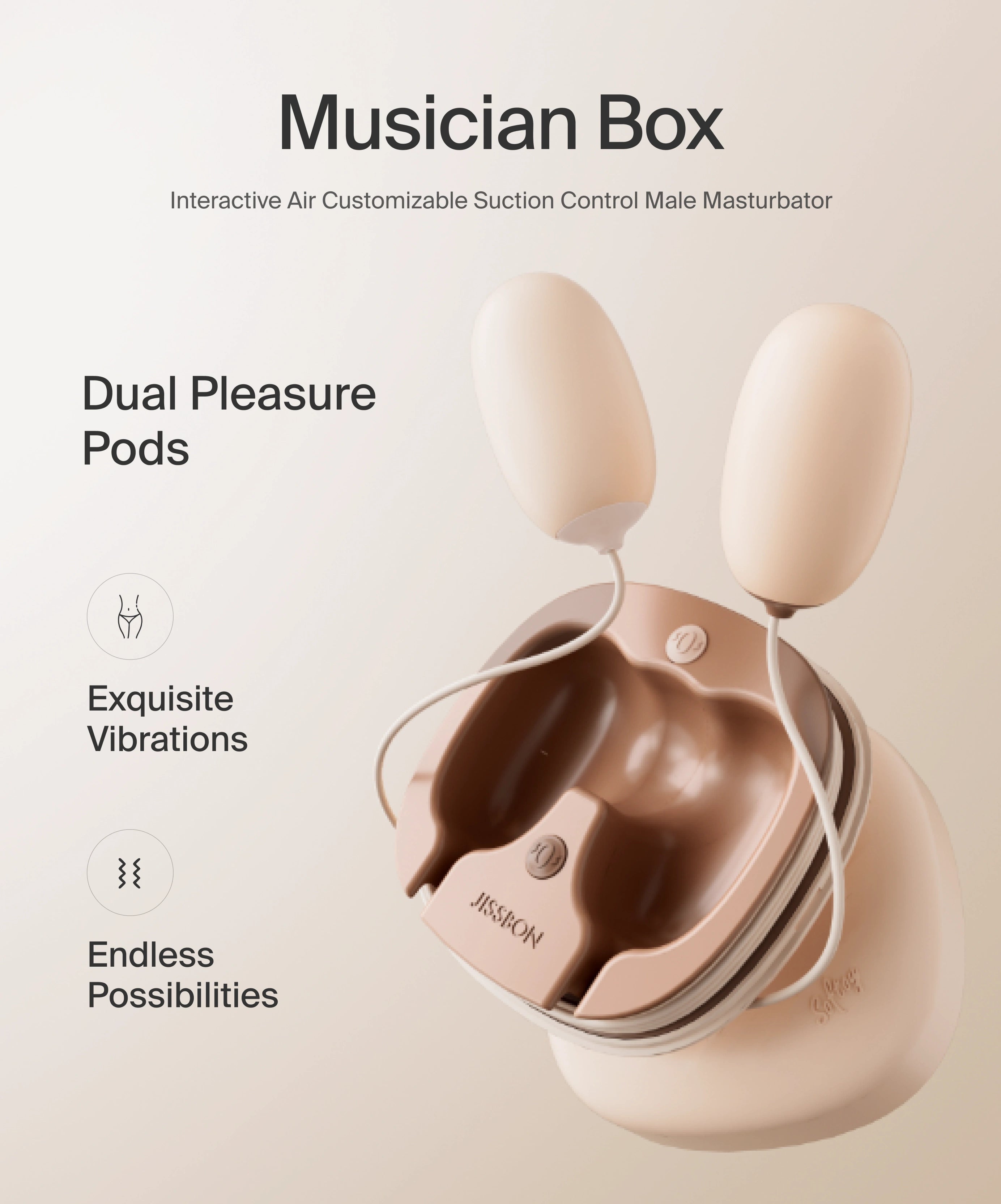
- Toy hygiene: wash toys with mild soap and warm water; dry fully. On sensitive days, stick to external stimulation with a soft bullet and lube.
Skip this (it backfires):
- Douching or “vaginal detox” products—disrupts flora and worsens burning.
- Scented washes/wipes or deodorant sprays anywhere on the vulva.
- DIY food remedies (yogurt/garlic/honey inside the vagina)—irritating and not sterile.
- Numbing creams on mucosa (mask pain → more microtears).
- Repeated OTC antifungals when you’re not sure it’s yeast (delays correct care).
Prevention: small habits, big comfort
- Lube like a pro. Friction is the #1 preventable cause of post-sex burning. Use enough water-based lube; reapply when drag appears.
- Rinse, not scrub. The vagina is self-cleaning. Wash the vulva with lukewarm water; if you use cleanser, choose unscented and gentle.
- Cotton underwear and quick changes after workouts or swims.
- Smart grooming. If shaving, use a new blade, shave with hair growth using slip, and avoid perfumes on freshly shaved skin.
- Condom/material check. If latex irritates, try polyisoprene/polyurethane; skip spermicides and intense warming/tingle lubes if sensitive.
When to see a doctor—don’t wait on these
- Fever, pelvic/side pain, or you feel systemically unwell
- Sores, blisters, or new rashes on the vulva
- Strong/fishy odor, green/gray discharge, or bleeding not due to menses
- Severe burning with urination, blood in urine, or back pain (possible UTI/kidney involvement)
- Persistent symptoms >48–72 hours despite gentle home care
- Recurrent episodes (≥3–4 times/year)
- Pregnant or immunocompromised and experiencing symptoms
Conclusion
Feeling like your pussy is hot or dealing with a burning vagina can be distracting at best and miserable at worst. The good news: most cases trace back to fixable culprits—friction, product irritation, tight/damp clothing, or common infections—and they respond well to simple, gentle steps. Start with the basics: reduce friction (lube, rest days), remove irritants (unscented everything, breathable fabrics), cool and soothe (compress/sitz), and practice good hygiene (no douching, clean toys). If there’s no discharge but burning, think about hormones, pelvic-floor tension, or dermatologic causes. And if symptoms persist, escalate quickly: the fastest way back to comfort is a clear diagnosis, not guesswork.
Above all, treat burning as information, not a verdict. Pain means “pause and adjust,” not “push through.” With small habit tweaks and timely care when needed, you’ll protect your tissues, your pleasure, and your peace of mind.
Frequently Asked Questions
What does it mean when your private part is hot?
If you’re aroused, a warm, flushed feeling is normal. Ongoing burning or stinging, especially with pee, odor, discharge, rash, or sores, points to irritation, infection, or skin issues—and deserves attention.
How can I reduce heat in my private area?
Cool compress 5–10 minutes, switch to loose cotton underwear, avoid friction for a day, and use water-based lube during sex. Rinse with lukewarm water; skip scented products and douching.
Is it normal for your vagina to burn?
Brief sensitivity after vigorous sex or grooming can happen, but persistent burning isn’t “normal.” Check for irritants/infections and see a clinician if it lasts >48–72 hours or comes with other symptoms.
How to stop vaginal burning fast at home?
Gentle rinse, cool compress, loose clothing, rest from penetration, and OTC pain relief if safe for you. If you suspect yeast and have classic symptoms you’ve had before, an OTC antifungal may help—otherwise, get tested.
Why is there burning but no discharge?
Think hormonal dryness, pelvic-floor tension, eczema/psoriasis/lichen, new products, or a UTI (which affects urine, not discharge). A clinician can sort this out with an exam and simple tests.
Can lube or condoms cause burning?
Yes—menthol/warming agents, flavors, dyes, or latex/spermicides can irritate. Try a non-latex condom and an unscented water-based or aloe-based lube with a short ingredient list.
Should I douche if I feel hot or dirty?
No. Douching disrupts natural flora and often worsens burning and odor. Rinse the vulva with lukewarm water and let the vagina (internal) self-clean.
Read more

If you’ve wondered, “why does my penis feel warm?”, you’re not alone. A warm or hot penis can be completely normal (think: blood rushing in when you’re aroused) or a sign that something needs atten...

Curious about the banana split sex position but not sure how to set it up without cramps or chaos? You’re in the right place. The banana split position is a playful mix of openness, angle control, ...