If you’ve wondered, “why does my penis feel warm?”, you’re not alone. A warm or hot penis can be completely normal (think: blood rushing in when you’re aroused) or a sign that something needs attention—like friction irritation, skin inflammation, or, less commonly, an infection. The tricky part is telling “normal heat” apart from burning, stinging, or pain that lingers after sex, workouts, or urination.
This guide breaks down the most common reasons for a warm sensation in the male groin area, what “penis burning” can mean, and what to do now—including simple home care that actually helps, plus clear red flags that mean it’s time to see a clinician. We’ll also cover prevention: smarter lube habits, breathable fabrics, safer grooming, and toy hygiene—because a lot of warm/burning episodes are fixable with small changes.
Use this as a calm, practical roadmap. If you have fever, severe pain, sores, discharge, or symptoms that don’t improve in a couple of days, skip the guessing and get checked. Otherwise, start here and work through the steps at your own pace.

Warm vs. burning: what’s normal and what’s not
A warm, flushed feeling during arousal is normal. Blood vessels dilate, the shaft and glans get warmer, and the skin can feel tight or tingly. That warmth should fade after stimulation and shouldn’t sting, itch, or hurt.
- Persistent heat or burning that lingers after sex or exercise
- Stinging with urination or after ejaculation
- Visible redness, rash, cracked skin, or swelling
- Discharge, unusual odor, or sores/blisters
- Fever, pelvic/side pain, or feeling unwell
Friction & environment: the most common (and most fixable) causes
Dry sex or long sessions: Without enough lubrication, repetitive motion creates microtears—tiny injuries that burn when you pee or shower. Solution: use plenty of water-based lube and reapply when drag shows up.
Tight, non-breathable clothes: Compression shorts, tight jeans, or sweaty underwear trap heat and moisture → chafing, heat rash, and folliculitis (inflamed hair follicles). Rotate in loose cotton or moisture-wicking underwear and change out of sweaty gear quickly.
Grooming & soaps: Freshly shaved or waxed skin + fragranced body wash = stinging and redness. If you shave, use a fresh blade, shave with slip (conditioner or lube), and rinse with lukewarm water. Stick to unscented cleansers and avoid scrubbing the glans/foreskin.
Sports & prolonged sitting: Cycling seats, long drives, and desk days compress the perineum and trap heat. Adjust bike fit, add breaks, and air things out.
What to do now: cool rinse or cool compress 5–10 minutes, loose underwear, rest from friction for 24–48 hours, and lube generously next time. If the skin is raw, a thin layer of a plain, fragrance-free emollient on intact skin can soothe.
Skin conditions that make the penis feel hot
Contact dermatitis (irritant/allergic): New detergent, scented wipes, menthol “tingle” products, latex condoms, or certain lubes can trigger redness, burning, and itch. Solution: stop the new product, rinse with lukewarm water, switch to unscented basics, try non-latex condoms, and choose a simple water-based lube with a short ingredient list.
Jock itch (tinea cruris): A fungal rash in the groin folds causes itch + warmth + redness with defined borders, often worse after sweating. OTC antifungal creams (per label) help, plus dry, breathable fabrics.
Balanitis (glans/foreskin inflammation): More common if uncircumcised: red, hot, tender glans, possible discharge or odor, burning with urination. Triggers include poor drying, harsh soaps, diabetes, or infections (yeast/bacteria). Gentle hygiene (retract, rinse, dry), avoid irritants, and see a clinician if it doesn’t settle in 1–2 days.
Eczema/psoriasis: Can affect the genital area and feel like burning or stinging. Requires tailored skincare and sometimes prescription treatment.
Infections & inflammatory causes (when “warm” feels like burning)
Urinary tract infection (UTI): Burning when you pee, frequency/urgency, lower abdominal discomfort; discharge is usually not prominent. Needs urine testing and antibiotics if confirmed.
Sexually transmitted infections (STIs): Chlamydia/gonorrhea can cause burning with urination and discharge; herpes can burn before blisters appear; trichomoniasis may cause irritation and odor. Testing is the only way to know—many STIs are asymptomatic.
Prostatitis (inflamed prostate): Pelvic/perineal ache, burning with urination, weak stream, pain with ejaculation, sometimes fever. This can be bacterial or non-bacterial; evaluation is key.
Epididymitis/orchitis: Testicular or epididymal pain/swelling with fever or urinary symptoms—urgent evaluation recommended.
Candidal (yeast) balanitis in men: Itchy/burning glans, redness, sometimes white patches—common after antibiotics, high heat/humidity, or with high blood sugar. Antifungals help; screen for diabetes if recurrent.

“Burning but no STD”: other explanations
- Dehydration & concentrated urine: Acidic urine stings if skin is already irritated. Hydrate well; a day of good fluids can help.
- Kidney stones or bladder irritation: Irritative urinary symptoms without infection can still burn; evaluation rules this in/out.
- Pelvic-floor tension: Overactive pelvic muscles can mimic urethral/prostate burning. Gentle stretches, diaphragmatic breathing, and pelvic-floor PT (if persistent) help.
- Medication/supplement effects: Some vitamins, caffeine, alcohol, and spicy foods can make urine sting more if skin is raw.
- Neuropathic pain: Less common, but nerve-based pain can feel like burning without visible skin changes.
What to do now (home care that actually helps)
- Cool, not hot: Rinse with lukewarm water, then use a cool compress (clean cloth) 5–10 minutes, 2–3 times on day one. Avoid ice directly on skin.
- Rest from friction: Pause penetrative sex or vigorous masturbation for 24–48 hours. When you resume, use plenty of lube and go slow.
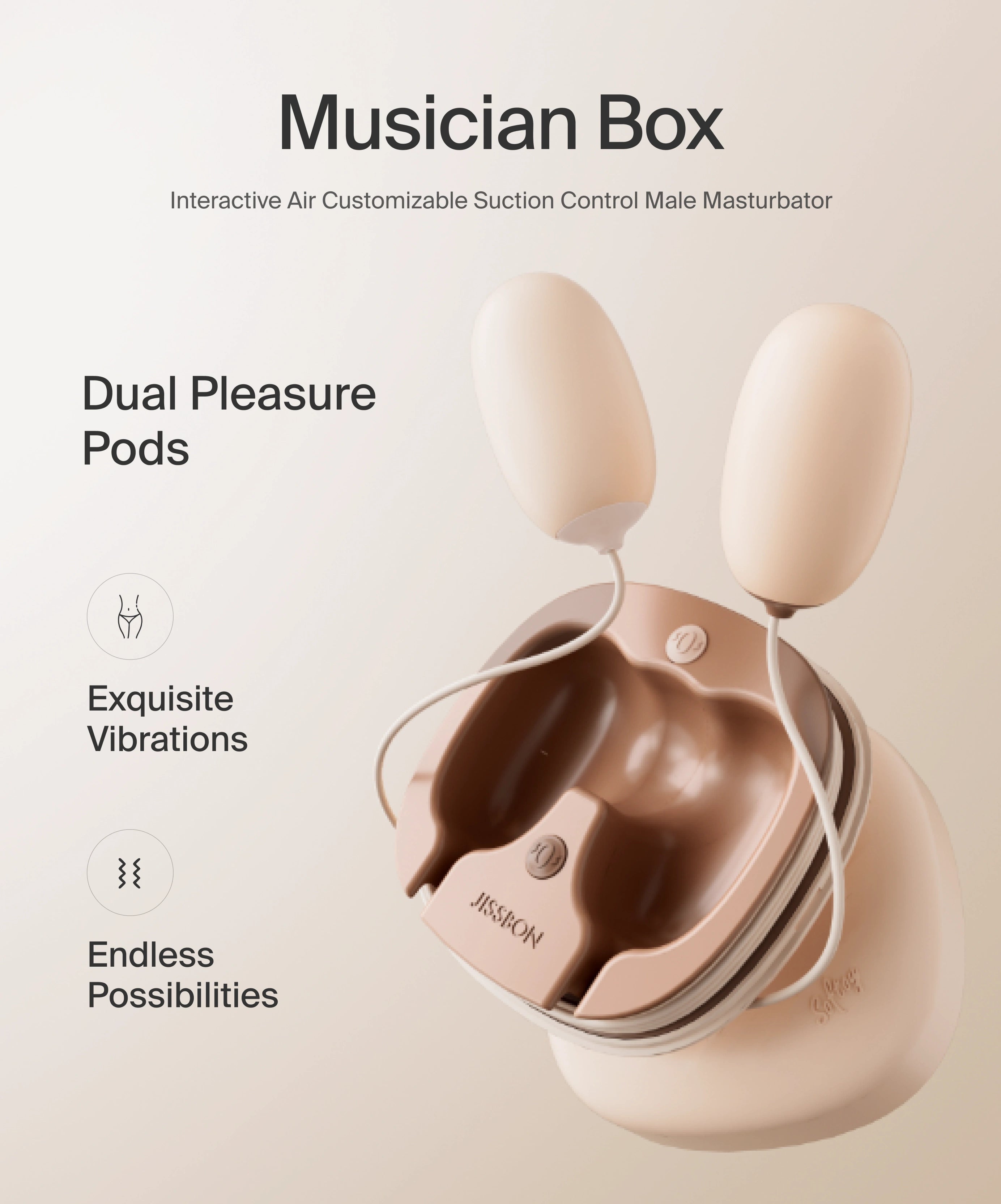
- Smarter lube: Choose a water-based lubricant for universal compatibility. Reapply when drag appears. If you’re using toys in the shower, silicone lube lasts longer—just avoid it directly on silicone toys unless you barrier it with a condom.
- Gentle hygiene: Retract foreskin (if present), rinse with water only, and pat dry—no scrubbing, no fragrances. Keep the area dry between skin folds.
- OTC where appropriate: If you suspect jock itch, try an OTC antifungal cream per label. For irritation, a tiny amount of 1% hydrocortisone on external skin (not mucosa) for a day or two can help—stop if worse; don’t use on open skin.
Prevention: small habits, big comfort
- Lube like a pro: Friction is the #1 preventable cause of post-sex burning. Keep a bottle within reach and reapply when needed.
- Breathe & pace: Short, steady strokes beat fast, dry motion. Take micro-breaks and check in with your body.
- Fabric & fit: Rotate in cotton or moisture-wicking underwear. Change out of sweaty clothes promptly. Avoid sleeping in tight compression shorts.
- Smart grooming: If shaving, use a fresh blade and shave with the grain; rinse gently; avoid fragranced products on freshly shaved skin.
- Condoms & lube ingredients: If latex bothers you, try polyisoprene or polyurethane condoms. Skip spermicides and intense warming/tingle lubes if you’re sensitive.
- Hydration & bathroom habits: Drink water through the day; don’t hold urine for long stretches—stagnant urine increases irritation risk.
- Regular screening: If you’re sexually active with new/multiple partners, regular STI screening catches issues early—even without symptoms.
When to see a doctor (don’t wait on these)
- Fever, chills, or you feel systemically unwell
- Discharge from the urethra, sores/blisters, or a spreading rash
- Severe burning with urination, blood in urine, flank/back pain
- Testicular pain/swelling (possible epididymitis/orchitis)
- Persistent symptoms >48–72 hours despite gentle care
- Recurrent episodes (3+ times in a year)
- You’re immunocompromised or have uncontrolled diabetes
Conclusion
A warm penis during arousal is normal; a burning or hot sensation that hangs around usually isn’t. Most cases trace back to friction, sweaty fabrics, or irritating products—and respond quickly to cooling, rest, and better lube/hygiene. When symptoms include stinging with urination, discharge, rash, sores, fever, or testicular pain, think beyond irritation: UTIs, balanitis, STIs, or prostatitis need proper testing and treatment—not guesswork.
Keep things simple: hydrate, rinse (don’t scrub), switch to breathable underwear, and lube generously during sex or masturbation. Clean toys and sleeves after use, and give your skin a day off when it’s irritated. If you’re unsure—or symptoms persist—see a clinician. Getting a clear diagnosis is the fastest way back to comfort and peace of mind.
Your body is giving you useful information. Listen, adjust, and you’ll protect both comfort and pleasure going forward.
Frequently Asked Questions
Why does my private part get warm?
During arousal, increased blood flow naturally warms the penis and surrounding skin. If the warmth comes with burning, stinging, rash, discharge, or fever, it’s more likely irritation or infection and deserves attention.
Why am I burning but no STD (men)?
Non-STD causes include friction, jock itch, balanitis, UTI, dehydration (acidic urine stinging irritated skin), pelvic-floor tension, or contact dermatitis from soaps, condoms, or lube ingredients. Testing rules out infection; prevention focuses on lube, fabrics, and gentler products.
Why is my peepee warm?
Urine is close to body temperature; if skin is irritated or you’re dehydrated (more concentrated urine), it can sting and feel extra warm. Hydrate and address skin friction/irritants.
Why is my pennis always wet?
Possible reasons: pre-ejaculate during arousal, sweat from tight clothing, urine drips after peeing, or urethral discharge from infection (especially if cloudy, yellow/green, or malodorous). If wetness is persistent or looks like discharge, get tested.
Why does my penis feel hot after sex or masturbation?
Usually friction. Use more water-based lube, shorten strokes, and take micro-breaks. If burning persists >48 hours or you see a rash, evaluate for dermatitis, jock itch, or balanitis.
Can condoms or lube make it burn?
Yes—latex, spermicides, menthol/warming agents, flavors, dyes, or certain glycols can irritate. Try non-latex condoms and an unscented water-based lube with a short ingredient list.
How do I stop burning fast at home?
Cool compress 5–10 minutes, rest from friction 24–48 hours, loose cotton underwear, gentle rinse only, and plenty of lube next time. If you suspect infection or symptoms persist, see a clinician.
Read more

If you’re asking what lube to use with sex toys, good news: the right lube dramatically improves comfort, sensation, and safety—and it’s easy to choose once you know a few rules. The best lube for ...

If you’re thinking “why is my pussy hot?” or you feel a burning vagina sensation, you’re not alone. Genital heat or burning can range from totally normal (increased blood flow when you’re turned on...