Short answer: “Clitoral atrophy” isn’t a stand‑alone diagnosis in most medical playbooks—it’s a visible/feelable change that often appears as part of genitourinary syndrome of menopause (GSM) or certain vulvar skin conditions. Because it’s usually one sign within a larger condition, there isn’t a single prevalence number for clitoral atrophy by itself.
What we can say: GSM symptoms affect roughly 27%–84% of postmenopausal women, and clitoral changes (thinning, reduced engorgement, hood tightness/adhesions) are routinely described within that spectrum.
In postpartum lactation—a temporary low‑estrogen state—GSM‑like symptoms are also reported. In specialty clinics, clitoral adhesions (a related structural issue) have been observed in about 23% of referred patients, underscoring that clitoral changes are not rare in symptomatic groups.
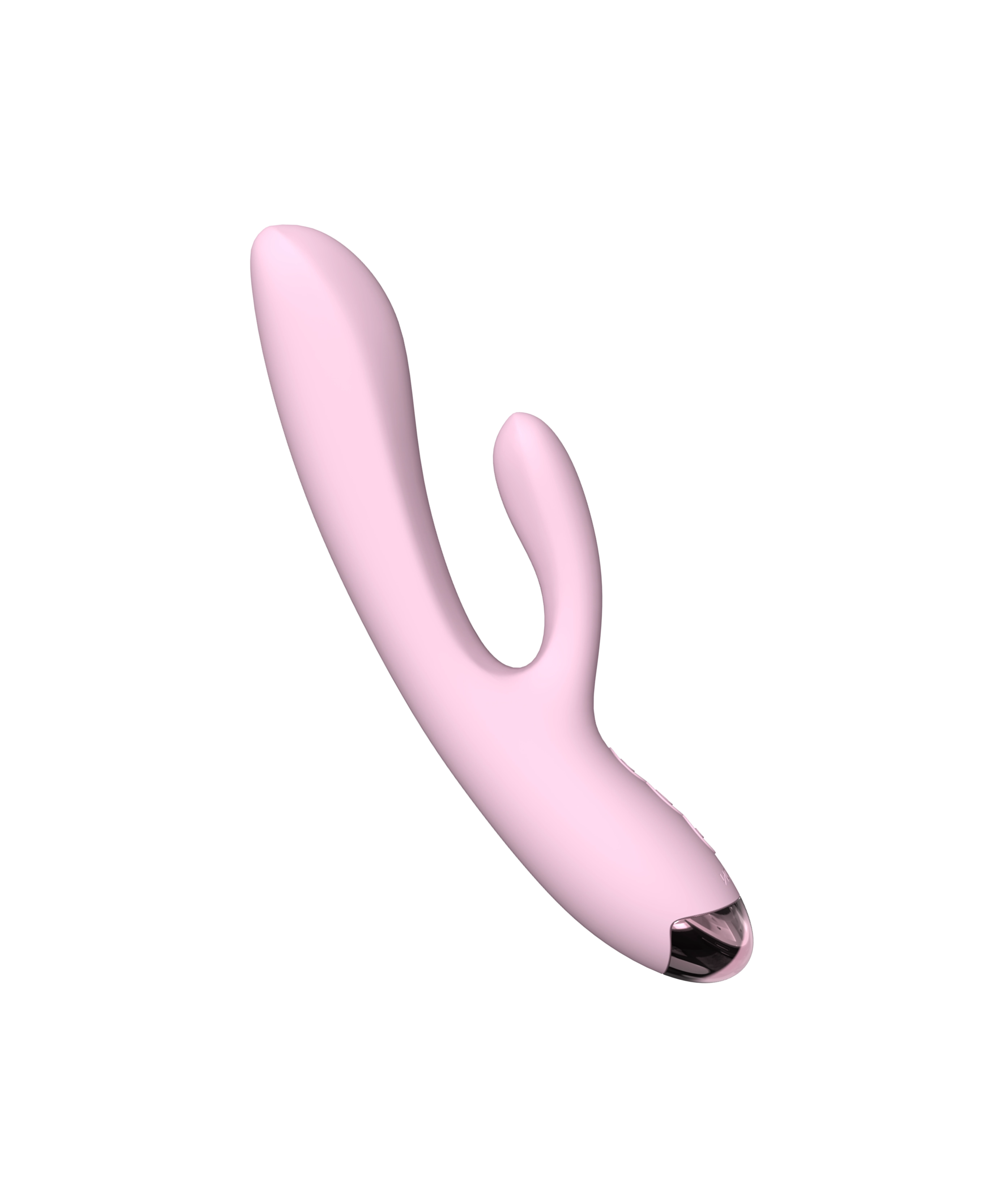
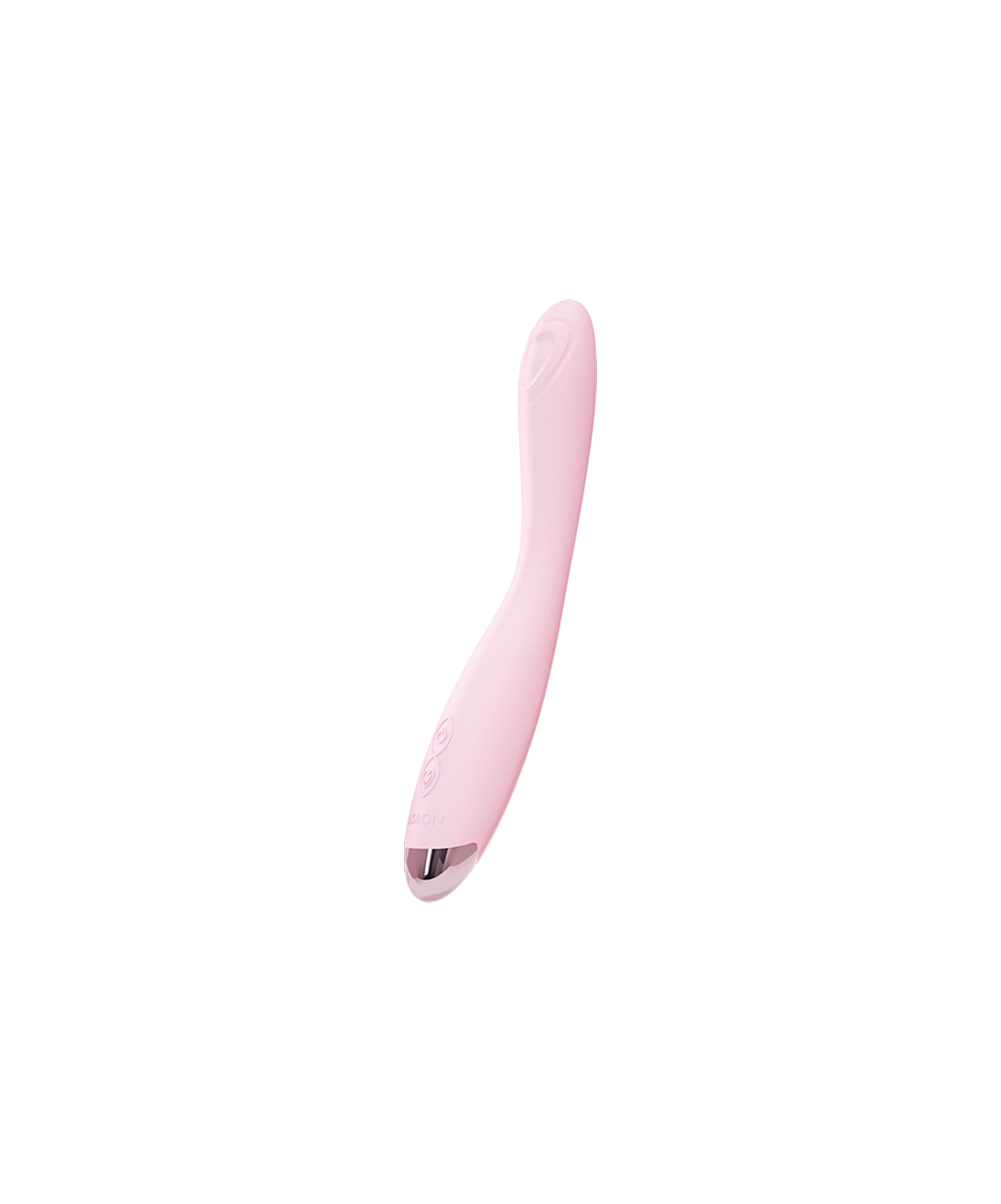
Looking for gentle, low‑friction ways to increase clit sensitivity while tissues recover? Explore clitoral vibrators—air‑pulse styles encourage blood flow with very light contact. A soft option like Miss Jelly Clitoral Suction Vibrator keeps stimulation comfortable while you address root causes.

What Is Clitoral Atrophy?
“Clitoral atrophy” describes thinning skin, reduced engorgement, decreased sensitivity, and sometimes hood tightness/adhesions that make the clitoris look or feel smaller (what many call “clitoris shrinking”). It commonly appears within GSM, the modern term for vulvovaginal/urinary changes driven by estrogen deficiency (most often after menopause, but it can occur in other low‑estrogen states). GSM is chronic and tends to progress without treatment.
Other conditions can mimic or contribute to clitoral atrophy—especially lichen sclerosus (LS), a chronic inflammatory skin disorder that can scar or fuse the clitoral hood. LS is underrecognized: population estimates range around 0.1%–0.3%, with higher prevalence (≈1.7%) reported in gynecology practices.
How Common Is Clitoral Atrophy?
Because “clitoral atrophy” is a sign, not a single coded diagnosis, epidemiology is inferred from related conditions:
- GSM prevalence: 27%–84% of postmenopausal women report GSM symptoms in reviews and guidelines. Clitoral changes are part of the vulvar exam findings in GSM.
- Postpartum/lactation (“genitourinary syndrome of lactation”): Studies and reviews note hypoestrogenism during breastfeeding can lead to dryness, pain, and GSM‑like changes; research is growing and prevalence varies by study.
- Clitoral adhesions (specialty data): In a vulvoscopy photo study from a tertiary practice, ~23% of patients had clitoral adhesions; this likely overestimates community prevalence, but it shows clinically significant clitoral change is not rare in symptomatic cohorts.
- Lichen sclerosus: Underdiagnosed overall; reports range 0.1%–0.3% in general settings, ~1.7% in gyne practices. LS can cause “clitoral phimosis” (hood fusion) and reduced sensitivity.
Clitoral Atrophy Symptoms
- Diminished engorgement or sensitivity
- Dryness, burning, itching, micro‑tears
- Hood tightness, difficulty retracting the hood; possible adhesions masking the glans
- Dyspareunia (pain with touch or penetration), difficulty reaching orgasm
- GSM‑associated urinary symptoms (urgency, frequency, dysuria, recurrent UTIs) may co‑occur
What Causes Clitoral Atrophy?
1) Low estrogen (GSM and other hypoestrogenic states)
Estrogen supports genital blood flow, thickness, and elasticity. Menopause is the most common cause, but postpartum/lactation, oophorectomy, and anti‑estrogen medicines (e.g., aromatase inhibitors, some breast cancer therapies) can produce similar changes.
2) Dermatologic disease
Lichen sclerosus scars and thins vulvar tissues and can fuse the hood over the clitoris (phimosis). It requires high‑potency topical steroids and regular follow‑up.
3) Adhesions & keratin pearls
When the hood sticks to the glans, adhesions may form; “keratin pearls” under the hood can cause pain and blunting of sensation. These are often detectable on exam and have office‑based treatments (see below).

Can Clitoral Atrophy Be Reversed?
Often—yes—if you treat the underlying cause. For GSM and other low‑estrogen states, local therapies are strongly supported; for skin disease, medical dermatologic care (and, selectively, minor procedures) can restore exposure and comfort.
- GSM treatments with evidence: Low‑dose vaginal estrogen, vaginal DHEA (prasterone), and oral ospemifene all improve at least some GSM symptoms. Multiple guidelines (NAMS 2020/2022; AUA/SUFU/AUGS 2025) and evidence reviews support these options. Expect initial relief within 2–6 weeks for local estrogen, with continued improvement over time. GSM tends to progress without ongoing therapy, so maintenance matters.
-
Adhesions/phimosis: If clitoral hood adhesions persist after medical therapy, in‑office lysis (freeing the hood and removing keratin pearls) has shown reduced pain and better sexual function in pre–post studies and patient‑reported series. Surgical correction in selected cases reports high satisfaction and low complication rates.
Special populations: If you have a history of estrogen‑dependent breast cancer, start with non‑hormonal care. If symptoms persist, ACOG supports shared decision‑making about low‑dose vaginal estrogen or prasterone in consultation with oncology.
Clitoral Atrophy Treatment: What Actually Works (Evidence‑Based)
First‑line comfort & non‑hormonal care
-
Vulvar moisturizers and lubricants (silicone or water‑based) reduce friction and micro‑tears.
- Hyaluronic acid (HA) gels: A 2024 pilot RCT found no clinically meaningful differences between vaginal HA and vaginal estrogen after 12 weeks—HA can be a promising non‑hormonal option, especially if hormones aren’t preferred.
- Pelvic floor physical therapy: Helpful if protective clenching worsens pain and sensitivity.
- Gentle stimulation to increase clit sensitivity: Regular, comfortable external stimulation (fingers or low‑intensity air‑pulse) can boost blood flow and comfort over time—supplemental to treating root causes. (See “At‑Home Plan” below.)
Local hormonal and SERM options (GSM)
- Low‑dose vaginal estrogen (cream, tablet, insert, ring): Strong evidence for dryness, pain, and exam signs of atrophy; minimal systemic absorption at low doses. Initial improvement often in 2–6 weeks.
- Vaginal DHEA (prasterone) 6.5 mg daily: Improves dyspareunia and tissue metrics via local conversion to estrogens/androgens.
- Ospemifene (oral SERM) 60 mg daily: Non‑estrogen option with RCT support for GSM symptoms (vaginal dryness, dyspareunia).
- Systemic menopausal hormone therapy (when indicated): For patients with broader menopausal symptoms where systemic therapy is appropriate, NAMS notes benefits for GSM as well.
Dermatology‑driven care
- Lichen sclerosus: Diagnose clinically (biopsy if unclear) and treat with ultra‑potent topical corticosteroids; long‑term maintenance is standard, with monitoring for scarring and rare malignancy.
- Clitoral adhesions/phimosis & keratin pearls: After addressing inflammation, in‑office lysis and removal of keratin pearls can reduce clitoral pain and improve orgasmic function in selected patients.
Not first‑line: energy‑based vaginal “rejuvenation”
Large guideline reviews (AUA/SUFU/AUGS 2025) report insufficient evidence that energy‑based devices outperform established therapies for GSM. Choose proven options first.

How Fast Will You Notice Changes?
- Moisture, comfort, less irritation: 2–6 weeks with local estrogen; similar timelines are reported for other evidence‑based GSM therapies.
- Sensitivity/sexual comfort: Gradual; depends on the cause (e.g., GSM vs. lichen sclerosus), consistent use of therapies, and gentle stimulation practices. GSM generally requires ongoing therapy to maintain gains.
At‑Home Plan to Increase Clit Sensitivity (Pairs with Medical Care)
- Daily barrier repair (2–3 min): Apply a vulvar moisturizer to outer tissues to reduce friction and micro‑tears.
- 3–4×/week stimulation (5–10 min): With lube, use light, non‑frictional touch at the hood edges or a low‑intensity air‑pulse vibrator. Keep sessions short and pleasant; stop if sore.
- Before sex: Use a long‑lasting lube and warm up externally for several minutes before direct clitoral contact.
- Every few weeks: Self‑check for white shiny patches, splits, or fused hood—see a clinician if present (possible lichen sclerosus or adhesions).
When to See a Clinician
- Pain, bleeding, or white shiny patches on the vulva/clitoral hood
- Hood won’t retract or the clitoris feels “stuck” (possible adhesions)
- Recurrent UTIs, burning with urination, or vaginal pain with dryness
- Post‑breast‑cancer GSM symptoms (discuss options with your oncologist + gynecologist)
- Little/no improvement after several weeks of moisturizers and gentle stimulation (you may need prescription therapy)
These can signal GSM that needs medical treatment or skin disease (e.g., lichen sclerosus) that requires topical steroids and follow‑up—and, occasionally, procedural treatment for adhesions.

Frequently Asked Questions
How common is clitoral atrophy?
There’s no single percentage because it’s a sign, not a standalone diagnosis. But the condition that most often includes it—GSM—affects ~27%–84% of postmenopausal women, and clitoral changes are part of the clinical picture. Clitoral adhesions show up in ~23% of patients in specialty clinics (not population‑wide).
Can clitoral atrophy be reversed?
Often, yes. Treat the cause: low‑dose vaginal estrogen, vaginal DHEA, or ospemifene for GSM; topical steroids for lichen sclerosus; and lysis of adhesions if a tight hood persists. Ongoing maintenance helps keep results.
What are the hallmark clitoral atrophy symptoms?
Less engorgement/sensitivity, dryness, hood tightness/adhesions, and pain with touch or sex—often alongside GSM urinary symptoms.
I’m breastfeeding—can I get clitoral atrophy?
You can experience GSM‑like symptoms (dryness, pain) due to lactation‑related hypoestrogenism. Discuss options with your clinician; many improve as hormones normalize or with targeted therapy.
Do “vaginal lasers” fix clitoral atrophy?
Guidelines say evidence is insufficient; stick with proven therapies first (local estrogen, DHEA, ospemifene, moisturizers, PT).
How fast will treatment work?
Some improvement can appear in 2–6 weeks with local estrogen; other therapies have similar timeframes. Sensitivity often improves gradually with consistent care.
What if my clitoris is covered or “stuck”?
That may be hood adhesions. Treat inflammation first; if exposure/sensation don’t return, in‑office lysis can help selected patients.
Read more

Short answer: Often—yes, clitoral atrophy can be improved or partly reversed—but it depends on the cause. When clitoral changes are part of genitourinary syndrome of menopause (GSM) or other low‑es...

Curious about a male anal orgasm but want a clear, safe, step‑by‑step guide? You’re in the right place. Below you’ll learn what a male anal orgasm feels like, how to find the prostate, beginner‑fri...