Short answer: Often—yes, clitoral atrophy can be improved or partly reversed—but it depends on the cause. When clitoral changes are part of genitourinary syndrome of menopause (GSM) or other low‑estrogen states, targeted treatments (like low‑dose local estrogen, vaginal DHEA, or ospemifene) can restore moisture, elasticity, and comfort, which may increase clitoral responsiveness and reduce pain. If the problem is skin disease (e.g., lichen sclerosus) or clitoral adhesions, topical steroid therapy and—in select cases—minor surgical lysis can uncover the glans and improve sensitivity. Because GSM is chronic and progressive without treatment, ongoing care matters for lasting results.
What Is Clitoral Atrophy?
“Clitoral atrophy” describes thinning, dryness, reduced engorgement, and sometimes hood tightness or adhesions that make the clitoris look or feel smaller (“clitoris shrinking”). It commonly occurs as part of GSM, the modern term for hormonally driven changes in vulvar, vaginal, and urinary tissues due to estrogen deficiency (menopause is the most common cause, but hypoestrogenism can also occur with lactation, anti‑estrogen medications, or ovarian removal). Clinical guidelines list clitoral atrophy among the physical changes seen with GSM.
Clitoral Atrophy Symptoms
People describe a mix of genital and sexual symptoms:
- Reduced clitoral swelling or decreased sensitivity
- Tight or stuck clitoral hood; difficulty finding the glans
- Dryness, burning, itching, micro‑tears
- Dyspareunia (pain with penetration or clitoral touch)
- Less lubrication and difficulty reaching orgasm
- Possible urinary symptoms (urgency, frequency, dysuria, recurrent UTIs) when GSM is present
What Causes Clitoral Atrophy?
Low estrogen (GSM & other hypoestrogenic states).
Estrogen maintains genital blood flow, thickness, and elasticity. Lower levels—in menopause, postpartum/lactation, hypothalamic amenorrhea, or from anti‑estrogen therapies (e.g., aromatase inhibitors for breast cancer)—thin tissues and reduce lubrication.
Dermatologic disease (especially lichen sclerosus).
Lichen sclerosus can scar or fuse the clitoral hood and shrink surrounding tissues. It needs potent topical steroids and follow‑up; adhesions sometimes require surgical release to restore exposure and sensation.
Medication & medical history.
Anti‑estrogens (tamoxifen, AIs), GnRH analogs, oophorectomy, and some chronic conditions (e.g., significant weight loss with low hormones) contribute to “clit atrophy” via estrogen depletion.
Postpartum/lactation.
Breastfeeding lowers estrogen and androgens, so temporary GSM‑like vulvovaginal changes—including dryness and pain—are common; many improve after lactation ends or with targeted therapy.

Can Clitoral Atrophy Be Reversed?
Often, yes—if you treat the underlying cause. For hypoestrogenism/GSM, local therapies have the strongest evidence:
- Low‑dose vaginal estrogen (cream, ring, tablet/insert) improves vaginal and vulvar symptoms (dryness, irritation, dyspareunia) and helps restore mucosal health; many patients report improved arousal and comfort around the clitoris as tissues recover. It’s a first‑line, ongoing treatment.
- Vaginal DHEA (prasterone) is FDA‑approved for dyspareunia from VVA/GSM; cells convert DHEA locally to estrogen/androgens and clinical trials show symptom improvement with daily 6.5 mg inserts.
- Ospemifene (oral SERM) reduces GSM‑related dyspareunia and dryness when hormones aren’t suitable or desired.
Where skin disease is the driver, treating lichen sclerosus can halt or partially reverse tissue changes; if clitoral phimosis/adhesions persist, surgical lysis has documented success in restoring clitoral exposure and sensation.
Evidence‑Based Treatment Options (From First‑Line to Specialist Care)
1) At‑home & non‑hormonal support
-
Regular vulvar moisturizers & on‑demand lubricants reduce friction and micro‑tears; hyaluronic acid can help some users.
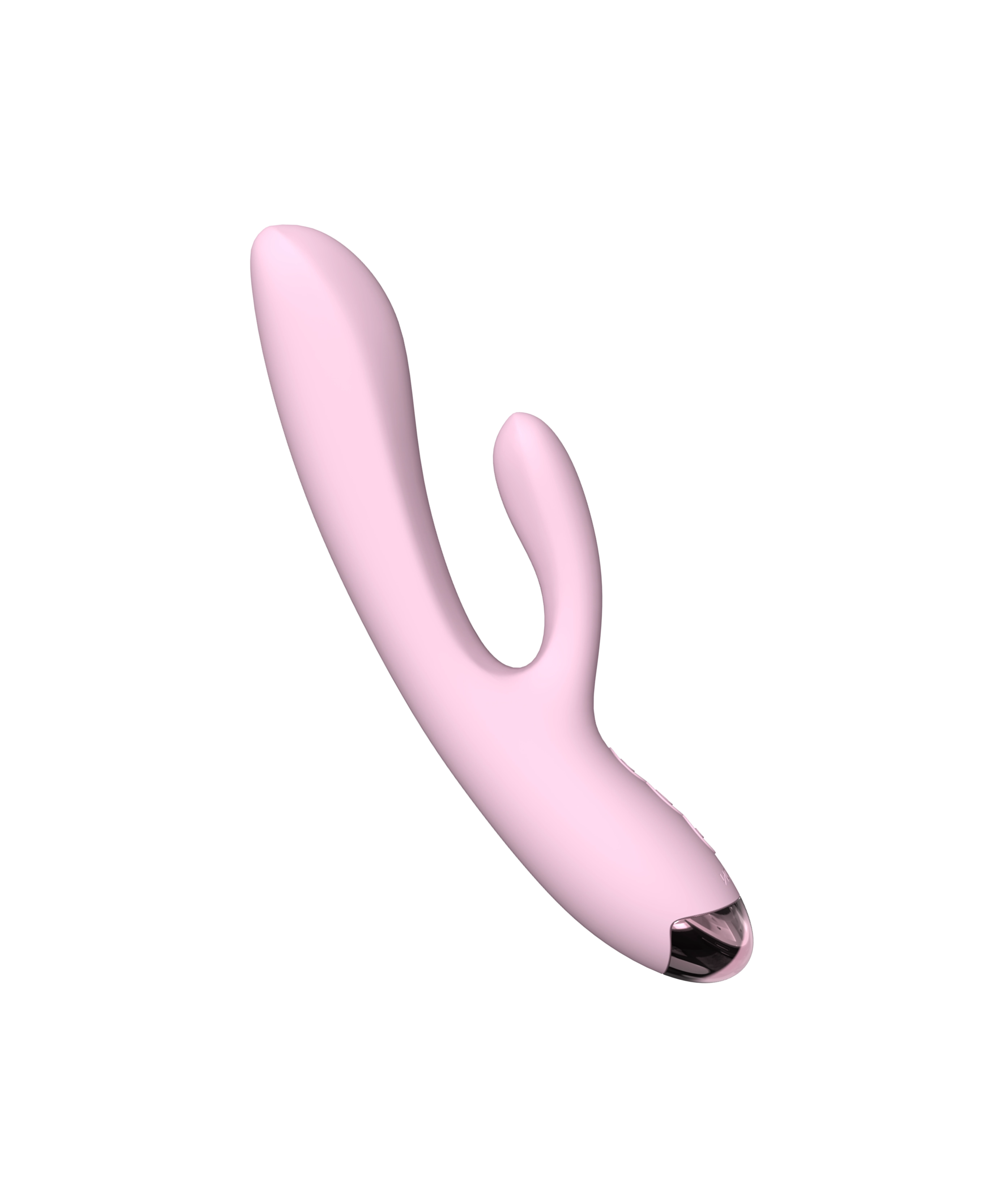
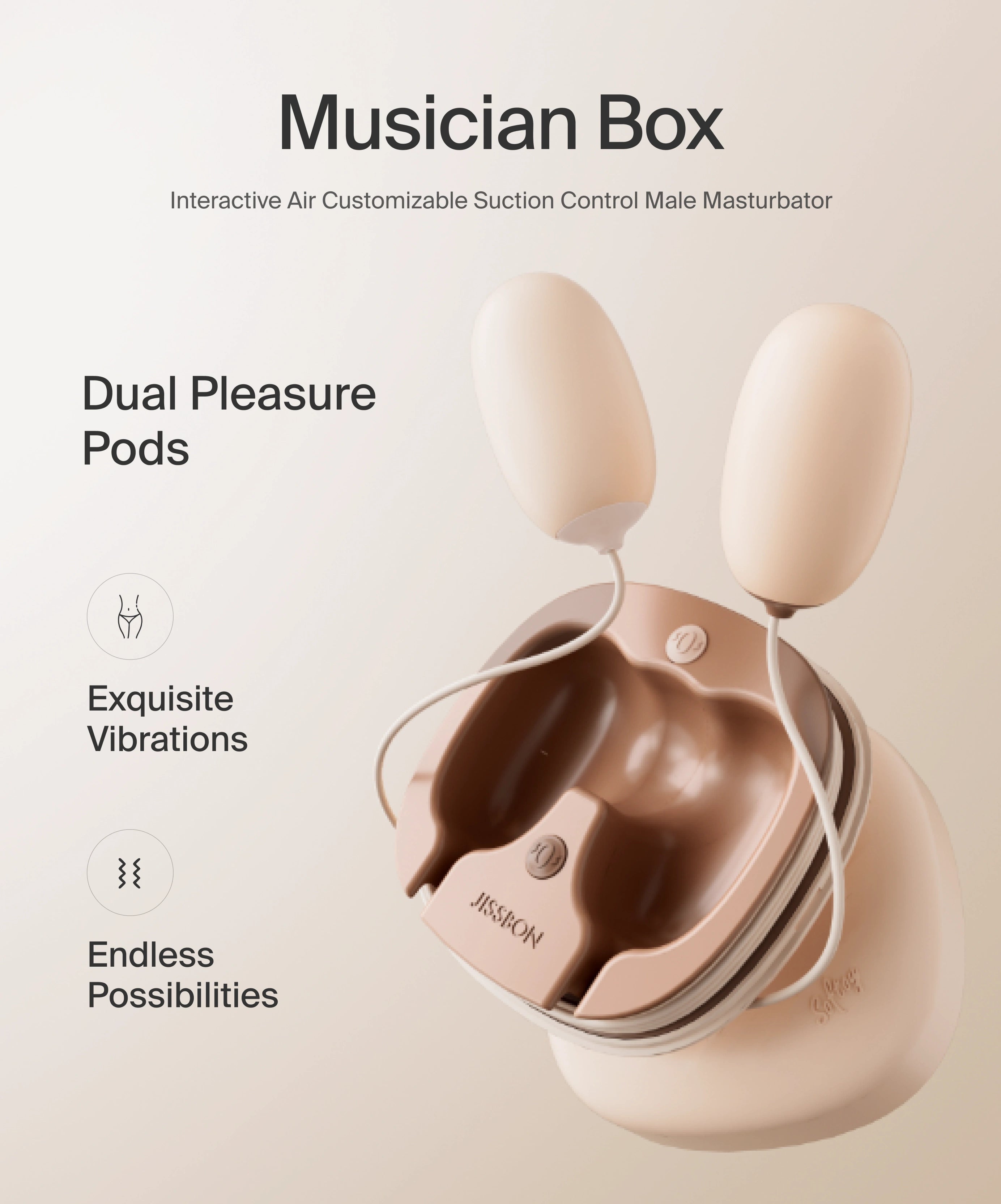
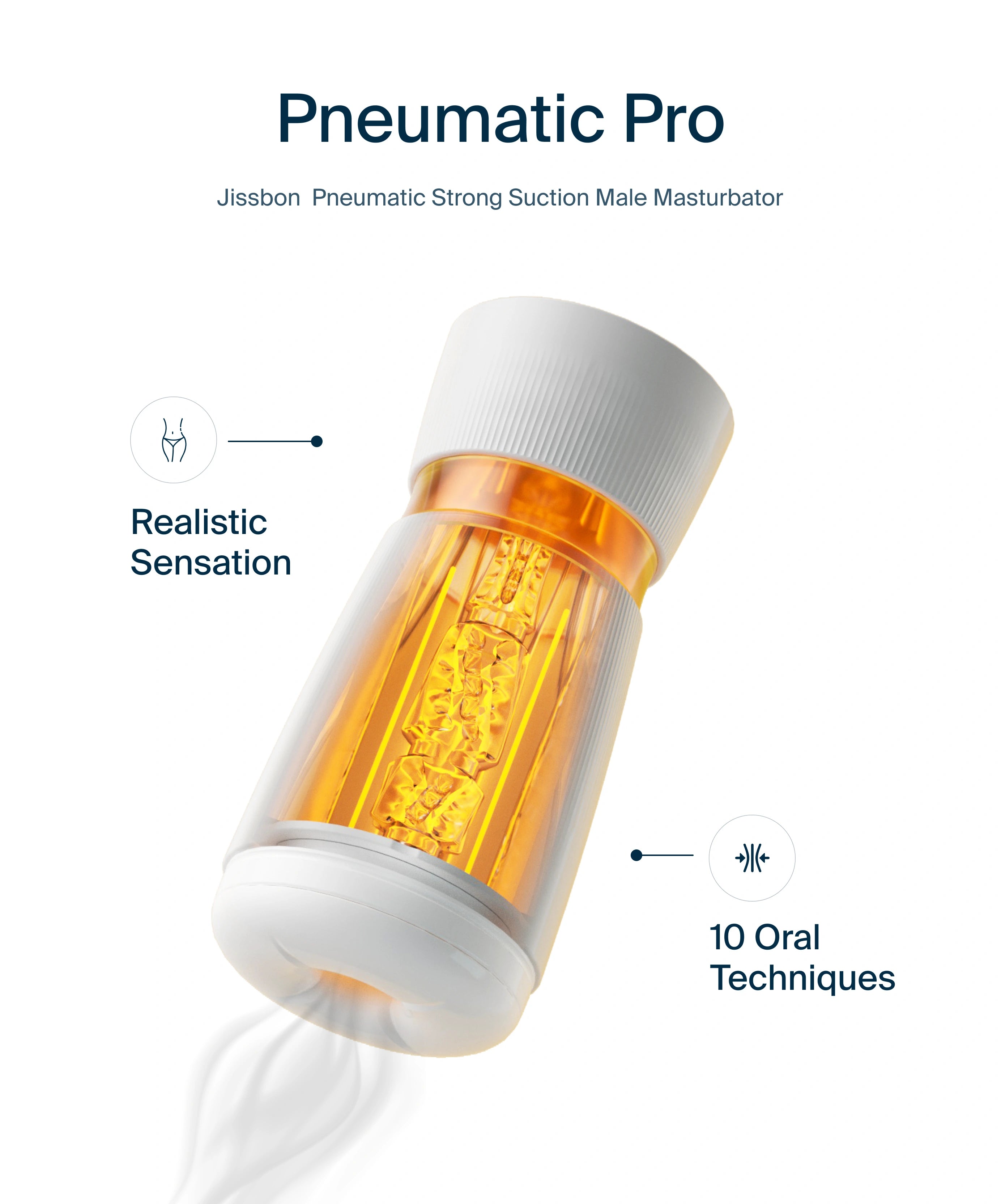
- Gentle clitoral stimulation (fingers or a soft vibrator) boosts blood flow and can increase clit sensitivity over time without abrasive friction. Sexual activity in general supports epithelial turnover and lubrication.
- Pelvic floor physical therapy can ease protective clenching and improve comfort with touch or penetration.
Want a precise, low‑friction option? Air‑pulse suction styles stimulate the clitoral complex without pressure on the skin—see clitoral vibrators or a soft starter like Clitoral Suction Vibrator.
2) Hormonal/local pharmacologic therapy (GSM)
- Low‑dose vaginal estrogen (cream, ring, tablet/insert): robust evidence for dryness, pain, and exam signs of atrophy; minimal systemic absorption at low doses. Apply as directed; many clinicians include the introitus/vulvar vestibule, and some advise a thin amount to the clitoral hood if tissue is pale and sore—follow your prescriber’s instructions.
- Vaginal DHEA (prasterone) 6.5 mg nightly: improved dyspareunia and tissue health; acts locally via intracrine conversion.
- Ospemifene 60 mg daily: an oral SERM for GSM‑related dyspareunia and dryness when local hormones are unsuitable.
- Systemic hormone therapy (HT): NAMS confirms HT is the most effective therapy for vasomotor symptoms and GSM in appropriate candidates; not needed if local therapy controls symptoms.
Special case—history of estrogen‑dependent breast cancer: Start with non‑hormonal measures. If symptoms persist, ACOG supports shared decision‑making about low‑dose vaginal estrogen or prasterone in consultation with oncology; many experts consider low‑dose local estrogen acceptable even years after cancer, but choices are individualized.
3) Treat dermatologic disease & adhesions
- Lichen sclerosus: Diagnose clinically/biopsy if unsure; treat with ultra‑potent topical corticosteroids (e.g., clobetasol) and long‑term maintenance; follow regularly due to small malignancy risk.
- Clitoral phimosis/adhesions: If pain or loss of function persists after medical therapy, manual or surgical lysis can reveal the glans and improve sensation with low complication rates.
4) What about “vaginal lasers” for atrophy?
Not recommended outside research: FDA has warned about marketing claims; major societies note insufficient evidence for GSM, and RCTs show mixed results. Choose proven therapies first.

How Long Until You Notice Changes?
- Moisture/comfort: often 2–6 weeks with local estrogen or prasterone; continue for full effect.
- Sexual comfort/sensitivity: gradual—depends on cause and consistency (e.g., daily moisturizers, regular external stimulation, pelvic PT). GSM typically requires ongoing therapy to maintain gains.
A Gentle At‑Home Plan to Increase Clit Sensitivity (Pairs Well With Medical Care)
- Daily (2–3 min): Apply a vulvar moisturizer to outer tissues to reduce micro‑irritation.
- 3–4×/week (5–10 min): With lube, use light, non‑frictional stimulation—fingertips at the hood edges or a soft air‑pulse device. Avoid aggressive suction.
- Before sex: Use a long‑lasting lubricant and warm‑up with external touch for several minutes before any direct clitoral contact.
- Every few weeks: Reassess comfort; if you see white patches, splits, fused hood, or pain, book an exam (possible lichen sclerosus/adhesions).
When to See a Clinician
- Pain, bleeding, or white shiny patches on the vulva/clitoral hood
- Hood won’t retract or clitoris seems “stuck”
- Recurrent UTIs with dryness/pain
- History of breast cancer and new GSM symptoms (discuss options with oncology + gynecology)
- Symptoms that don’t improve with moisturizers and gentle stimulation after a few weeks
These can signal GSM that needs prescription therapy or dermatologic disease that requires steroids and follow‑up—and, occasionally, procedural treatment.

Frequently Asked Questions
Can clitoral atrophy be reversed?
Often, yes—especially when it’s due to low estrogen (GSM) or treatable skin disease. Local estrogen, vaginal DHEA, or ospemifene can restore tissue health and comfort; lichen sclerosus responds to topical steroids, and adhesions can be released if needed. Ongoing maintenance matters.
What is clitoral atrophy?
A set of changes—thinning, dryness, reduced engorgement, possible hood adhesions—that can make the clitoris look smaller (“clitoris shrinking”) and feel less sensitive. It’s often part of GSM.
How fast will treatment work?
Some relief (moisture, less irritation) appears in 2–6 weeks with local therapies; sensitivity and comfort continue to improve with consistent use and gentle stimulation.
Is local estrogen safe if I had breast cancer?
Non‑hormonal options come first. If symptoms persist, ACOG supports shared decision‑making about low‑dose vaginal estrogen or prasterone with oncology input.
Do clitoral pumps reverse atrophy?
Evidence is limited. Gentle suction or air‑pulse devices may enhance blood flow temporarily, but over‑suction can bruise sensitive tissue. Use lube, go low, and stop if sore. (Address the root cause—often GSM—for lasting change.)
Are vaginal lasers a good fix?
Not first‑line. Major societies and the FDA cite insufficient evidence and potential risks; choose proven therapies like local estrogen, DHEA, moisturizers, and PT.
Can you learn to feel more?
Yes—steady, low‑friction stimulation, optimized lube, and pelvic PT (if you’re guarding or tense) can support sensitivity while medical treatments restore tissue health.
Read more

Understanding how to finger asshole properly is essential for safe, comfortable anal exploration. Whether you're curious about solo play or want to introduce anal fingering with a partner, the righ...
Short answer: “Clitoral atrophy” isn’t a stand‑alone diagnosis in most medical playbooks—it’s a visible/feelable change that often appears as part of genitourinary syndrome of menopause (GSM) or ce...