A post op trans vagina is the result of gender-affirming vaginoplasty, a surgical procedure that constructs vaginal anatomy for transgender women. Understanding recovery, maintenance, and sexual function helps you navigate this life-changing transition with confidence.
This guide covers anatomy, healing timelines, dilation practices, sexual exploration, and practical tips for reclaiming intimacy. Whether you're preparing for surgery, currently recovering, or supporting someone through this journey, you'll find evidence-based information presented clearly and compassionately.
Types of Vaginoplasty Techniques & How They Affect Healing
Different surgical methods create slightly different anatomy, lubrication behavior, and healing timelines.
1. Penile Inversion Vaginoplasty (Most Common)
- Uses penile skin to create vaginal canal
- Scrotal skin forms labia majora/minora
- Clitoris formed from glans with preserved nerves
Pros: reliable sensation, strong aesthetic results
Cons: requires lubrication for sex; depth varies based on available skin
2. Penile Inversion With Scrotal Graft
Adds additional scrotal skin to increase canal depth.
Pros: deeper canal
Cons: higher risk of granulation tissue
3. Intestinal Vaginoplasty (Sigmoid colon technique)
Portion of intestine forms the vaginal canal.
Pros: natural moisture, less dilation needed
Cons: longer surgery, abdominal scars, mucous discharge
4. Peritoneal Vaginoplasty (Newer technique)
Uses peritoneal lining inside the abdomen.
Pros: self-lubricating, long-term softness, minimal hair growth
Cons: requires laparoscopy, higher surgical complexity
Neovaginal Microflora: Cleaning, Douching & Odor Prevention
Unlike cis vaginas, a penile skin–lined neovagina:
- does not self-regulate pH
- does not produce lactobacilli
- can accumulate sweat, lubricant, and dead skin cells
Daily Hygiene Guidance
- Clean the vulva with warm water and mild, fragrance-free soap
- Gently rinse inside canal with warm water if recommended by your surgeon
- Avoid harsh soaps or scented washes
- Pat dry thoroughly—moisture causes odor and irritation
Douching (if instructed)
Mayo Clinic + TransCare BC note that some patients must rinse internally:
- Start around week 3–6 (surgeon-dependent)
- Use sterile saline or warm water only
- Never use over-the-counter scented douches
Odor Management
Common and normal early in recovery. Reduce odor by:
- thorough dilation cleaning afterward
- switching to water-based lubricant
- wearing breathable cotton underwear
- rinsing gently after sweating or intercourse
Who This Guide Serves
Gender-affirming surgery impacts multiple aspects of life, and accurate information helps everyone involved:
- Trans women considering vaginoplasty who want realistic expectations about outcomes and recovery
- Post-operative individuals navigating the first months and years of healing and adjustment
- Partners of trans women seeking to understand anatomy, function, and how to provide supportive intimacy
- Healthcare providers looking for patient-centered perspectives on post-surgical experiences
- Anyone exploring gender transition and evaluating whether bottom surgery aligns with their goals
- Friends and family members wanting to offer informed, compassionate support
Understanding Post-Surgical Anatomy

Vaginoplasty creates functional anatomy with multiple components working together.
Primary Structures Created
The surgical process constructs a vaginal canal, typically 5-6 inches deep, using penile and scrotal tissue or sometimes intestinal grafts. The clitoris forms from the glans with preserved nerve sensation. Labia majora and minora develop from scrotal and penile skin respectively.
A clitoral hood protects the sensitive clitoral tissue, while the vaginal opening sits between the labia. The urethra is repositioned for typical female urination positioning.
How It Functions
According to medical research on vaginoplasty outcomes, most surgical techniques preserve erectile tissue in the clitoris, maintaining capacity for arousal and orgasm. The vaginal canal doesn't self-lubricate naturally the way cisgender vaginas do, requiring external lubricant for comfortable penetration.
Nerve sensation varies by individual and surgical technique. Many people report pleasurable sensation throughout the vulva, with the clitoris typically most sensitive. The vaginal canal may have limited internal sensation initially, though some develop increased sensitivity over time.
Visual Appearance
Post-operative anatomy varies significantly between individuals, just as cisgender vulvas do. Factors affecting appearance include surgeon technique, body's natural tissue characteristics, healing patterns, and scarring.
Most surgical results look similar to cisgender anatomy once fully healed, though some scarring remains visible. Labia size, clitoral prominence, and overall configuration differ person to person. There's no single "correct" appearance—diversity is normal and expected.
Recovery Timeline: What to Expect
Healing happens in distinct phases, each with specific care requirements.
|
Phase |
Timeline |
Key Milestones |
Primary Focus |
|
Immediate Post-Op |
Days 1-7 |
Hospital stay, initial swelling, catheter removal |
Pain management, wound monitoring |
|
Early Recovery |
Weeks 2-6 |
Begin dilation, limited mobility, follow-up appointments |
Preventing infection, starting dilation routine |
|
Active Healing |
Months 2-6 |
Increased activity, establishing dilation schedule |
Building stamina, managing discomfort |
|
Stabilization |
Months 6-12 |
Reduced swelling, improved sensation, considering sexual activity |
Transitioning to maintenance dilation |
|
Long-Term |
Year 1+ |
Final appearance emerges, sensation continues developing |
Maintaining depth, enjoying normal activities |
First Two Weeks: Expect significant swelling, bruising, and discomfort. Most people stay 3-7 days in the hospital. You'll have packing removed (uncomfortable but brief), catheter typically stays 5-10 days, and movement is limited to prevent stress on sutures.
Months One Through Three: Swelling decreases noticeably. You'll dilate multiple times daily—initially 3-4 sessions of 15-30 minutes each. Returning to work depends on job requirements; desk jobs may be possible at 6-8 weeks, while physical labor requires longer recovery.
Six Months to One Year: Major healing completes, though subtle changes continue. Dilation frequency typically reduces to once daily or every other day. Sexual activity becomes more comfortable as tissues strengthen and you learn your body's responses.
Dilation: Essential Maintenance Practice

Regular dilation prevents vaginal stenosis (narrowing) and maintains depth achieved during surgery.
Why It's Necessary
Unlike cisgender vaginas, surgically created vaginal canals will narrow and shorten without regular use or dilation. The body treats the space as a wound trying to close. Consistent dilation "teaches" tissues to maintain the canal.
Equipment You'll Need
Surgeons provide initial dilator sets—usually 3-5 graduated sizes from pinky-finger width to average penis girth. These are typically medical-grade silicone or acrylic. You'll also need:
- Water-based lubricant (never silicone-based, which degrades silicone dilators)
- Clean towels
- Mild antibacterial soap
- Private, comfortable space where you can recline
Step-by-Step Dilation Process
- Preparation: Wash hands thoroughly and clean the dilator with antibacterial soap and warm water. Apply generous lubricant to the dilator and vaginal opening.
- Positioning: Lie on your back with knees bent and feet flat, or recline at 45 degrees with pillows supporting you. Some people prefer lying on their side.
- Insertion: Angle the dilator slightly toward your tailbone initially, then straighten as it enters. Apply gentle, steady pressure—never force it. The first inch is typically tightest.
- Maintenance: Once fully inserted, hold for the prescribed duration (usually 15-30 minutes). Some people read, watch shows, or meditate during this time.
- Removal: Gently pull straight out. Clean the dilator immediately and store in a clean, dry place.
Frequency Guidelines
According to post-operative protocols from gender-affirming surgery centers, typical schedules are:
- Months 1-3: 3-4 times daily
- Months 4-6: 2-3 times daily
- Months 7-12: 1-2 times daily
- After year one: 2-3 times weekly minimum
Penetrative sex counts as dilation, potentially reducing needed sessions.
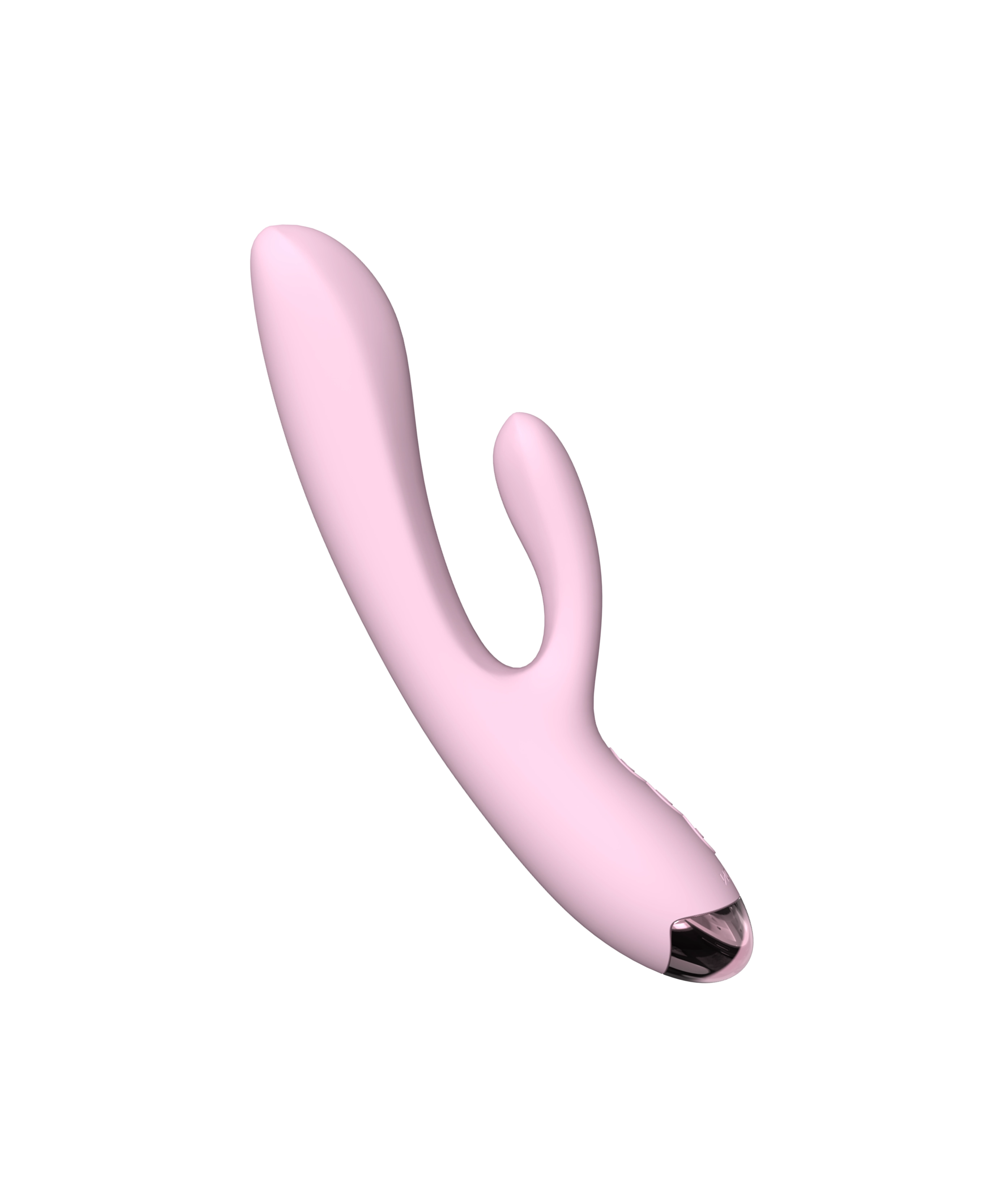
For those finding standard dilators uncomfortable or boring, some turn to graduated sex toys for women designed with smooth, body-safe silicone. Slim, tapered vibrators can serve dual purposes once cleared for sexual activity.
Sexual Function & Pleasure After Surgery
Understanding what's possible helps set realistic expectations while discovering your body's new responses.
Capacity for Orgasm
Most surgical techniques preserve the dorsal nerve bundle that provides clitoral sensation. Research indicates 70-90% of post-operative trans women report ability to reach orgasm, though the sensation may differ from pre-surgery experiences.
Arousal patterns often shift. Some people find their responsive desire increases—meaning arousal builds more from stimulation than spontaneous desire. Others discover new erogenous zones or different rhythms that work better post-surgery.
Lubrication Requirements
Surgically created vaginas don't produce natural lubrication. Always use lubricant for penetration, whether with toys, partners, or dilators. Water-based formulas work with all toy materials and condoms. Consider thicker, longer-lasting formulas for extended sessions.
Some people experience residual moisture from mucous membranes (especially with intestinal graft techniques), but it's typically insufficient for penetration without supplementation.
When to Start Sexual Activity
Most surgeons clear patients for masturbation around 6-8 weeks and penetrative activity at 10-14 weeks, though timelines vary by individual healing. Don't rush—premature activity risks tearing delicate healing tissues.
Start with external stimulation first. A gentle clitoral vibrator on low settings helps you discover what sensations feel pleasurable. Once cleared for penetration, begin with the smallest dilator size or slim toys before progressing.
Choosing Appropriate Toys for Exploration

The right products enhance comfort and pleasure during post-surgical exploration.
Size Considerations
Start smaller than you think necessary. What accommodates during clinical dilation doesn't always feel comfortable during arousal-focused activity. Slim bullet or finger-sized vibrators work well initially.
Gradually progress to girthier options as comfort allows. Rabbit vibrators with adjustable positioning let you control depth and clitoral contact simultaneously.
Material Safety
Body-safe silicone remains the gold standard—non-porous, easy to clean, and hypoallergenic. Avoid jelly rubber or porous materials that harbor bacteria. Quality brands like Jissbon prioritize medical-grade materials that meet post-surgical hygiene needs.
Feature Preferences
- Waterproof designs: Enable easy cleaning and bath/shower use during recovery when immersion may be limited
- Multiple speeds: Let you start gentle and build intensity as sensation develops
- Curved tips: Help target specific areas once you understand your internal anatomy
- Remote control options: Useful if reaching is uncomfortable during early recovery
Dual-Purpose Tools
Some products work for both maintenance and pleasure. Slim, graduated dilators with vibration functions serve clinical needs while adding enjoyable stimulation. This can make dilation routines less tedious and more connected to pleasure rather than medical obligation.
Common Challenges & Practical Solutions
Most post-operative individuals encounter similar obstacles. Here's how to navigate them effectively.
Dilation Discomfort or Pain
If insertion hurts beyond mild pressure, don't force it. Try relaxation breathing—tension tightens pelvic floor muscles. Use more lubricant than seems necessary. Consider dropping to the next smaller size temporarily.
If pain persists, consult your surgeon. You might have granulation tissue (excess healing tissue) requiring minor in-office treatment, or pelvic floor physical therapy may help release tight muscles.
Loss of Depth
If you've skipped dilation sessions and notice difficulty reaching previous depth, don't panic. Resume regular dilation with slightly longer sessions. Depth often returns within 1-2 weeks of consistent practice.
To prevent this, set phone reminders for dilation times. Many people treat it like medication—non-negotiable daily maintenance.
Limited Sensation
Nerve regeneration continues for 12-24 months post-surgery. If you're not experiencing much sensation early on, patience often resolves it. Some areas may never develop strong sensation—this varies individually.
Experiment with different types of touch: vibration, pressure, temperature play, rhythmic tapping. You might discover unexpected pleasure points. External stimulation on the clitoris, labia, and perineum often provides more sensation than deep vaginal penetration.
Emotional Adjustment
Having the anatomy you've always wanted doesn't automatically resolve all dysphoria or create instant sexual confidence. Some people experience unexpected grief, adjustment challenges, or continued body image struggles.
This is normal and doesn't mean surgery was wrong for you. Many find therapy specifically focused on sexual identity and post-surgical adjustment helpful. Support groups connecting you with other post-operative trans women provide community understanding that cisgender therapists may not offer.
Partner Communication & Intimacy Building
Navigating sexual connection after surgery requires openness and patience from everyone involved.
Before First Encounters
Discuss expectations, boundaries, and concerns when not in a sexual context. Share what you know about your body's responses and what remains uncertain. Establish signals for "more," "different," or "stop."
Many people feel vulnerable showing new anatomy to partners. Remember that any partner worth your time will approach with respect, curiosity, and care—not judgment.
During Exploration
Go slowly, with abundant lubrication and frequent check-ins. Your partner should ask questions: "Does this feel good?" "More pressure or less?" "Different angle?"
Voice your experience even when it's uncertain: "I'm not sure yet, let's keep trying" is perfectly valid. Silence can make partners anxious they're doing something wrong.
Adjusting Expectations
Both partners may have fantasies about post-surgery sex that don't match reality. Penetration might not be the main event—clitoral stimulation, full-body touch, or oral sex might provide more pleasure initially (or always).
For products that enhance partnered intimacy, sex toys for couples designed for multiple-person play can take pressure off penetration being the only route to pleasure.
Long-Term Care & Maintenance
After the first year, maintenance becomes routine rather than consuming.
Ongoing Dilation Schedule
Post-year-one, most people dilate 2-3 times weekly. If you're sexually active with regular penetration, you might reduce to weekly or as-needed. Listen to your body—if insertion becomes difficult, increase frequency temporarily.
Annual Check-Ups
Continue seeing your surgeon or a gynecologist familiar with post-operative trans anatomy annually. They check for prolapse (rare but possible), stenosis, unusual discharge, or other concerns.
Standard cervical cancer screenings don't apply since surgically created vaginas lack a cervix. However, if any original prostate tissue remains, that requires monitoring.
Pelvic Floor Health
According to guidance from pelvic health specialists, pelvic floor physical therapy benefits many post-operative individuals. It addresses tension, improves control, and can enhance sexual sensation.
Frequently Asked Questions
Does a post-op trans vagina look the same as a cis vagina?
Often very similar, especially after 6–12 months once swelling resolves. There is natural anatomical variation among cis and trans women, so “normal” includes a wide range of appearances.
Do you have to dilate for the rest of your life?
Most people need lifelong maintenance dilation, though frequency decreases dramatically. Regular penetrative sex may substitute for some sessions.
Can a trans woman have a natural orgasm after vaginoplasty?
Yes. Most techniques preserve clitoral nerves, allowing orgasm through external stimulation. Many report orgasms equal to or more satisfying than pre-surgery due to reduced dysphoria.
Does a trans vagina self-lubricate?
Penile inversion vaginas do not self-lubricate. Peritoneal or intestinal vaginoplasty may produce natural moisture, but most still require additional lubricant.
What does a fully healed post op trans vagina look like?
Appearance varies widely between individuals, similar to cisgender vulvas. Once swelling resolves (6-12 months), most results closely resemble cisgender anatomy with labia, clitoral hood, and vaginal opening. Scarring is typically minimal and fades over time. Surgeon skill and individual healing characteristics affect final appearance significantly.
Can you get wet naturally after vaginoplasty?
Most vaginoplasty techniques don't create self-lubricating tissue. Some people experience minor moisture from mucous membranes, especially with intestinal graft methods, but external lubricant is always necessary for comfortable penetration. This differs from cisgender vaginas and requires planning ahead for sexual activity.
How deep is the vaginal canal after surgery?
Typical depth ranges from 5-7 inches, varying by surgical technique and individual anatomy. This accommodates most partners comfortably. Maintaining achieved depth requires regular dilation or penetrative activity. Without maintenance, some narrowing and shortening occurs over time.
Does sex feel good after gender-affirming surgery?
Most people report pleasurable sensations, though experiences vary. Clitoral sensation usually remains strong since nerve preservation is standard. Vaginal canal sensation develops over 12-24 months as nerves regenerate. Many describe orgasms as different from pre-surgery but equally or more satisfying, especially as dysphoria decreases.
How often do you need to dilate long-term?
After the first year, 2-3 times weekly typically maintains depth and width. If you engage in regular penetrative sex (weekly or more), you might reduce to as-needed. Skipping months causes narrowing that requires intensive re-dilation. Think of it like exercise—consistency prevents backsliding.
What are the biggest challenges in the first year?
Consistent dilation proves most difficult for many—it's time-consuming and occasionally uncomfortable. Emotional adjustment to new anatomy, managing expectations about sensation and function, navigating first sexual experiences, and dealing with potential complications like granulation tissue also challenge people. Strong support systems help significantly.
Conclusion
Navigating post-operative life as a trans woman involves learning new anatomy, maintaining vaginal health through dilation, and discovering what pleasure feels like in your affirmed body. With patience, proper care, and supportive resources, most people develop satisfying sexual function and renewed intimate confidence.
Ready to explore pleasure in your body with thoughtfully designed, body-safe products? Discover options at sex toys for women created with diverse bodies and needs in mind.