Short answer: For most people, clitoral atrophy isn’t permanent. The clitoris itself doesn’t “disappear,” but the glans can look smaller, feel less sensitive, or seem hidden under the hood when hormones drop, blood flow decreases, or a skin condition causes adhesions.
With the right plan—moisturizers and lubricants, low‑dose vaginal hormones (when appropriate), gentle stimulation, and treatment of skin conditions like lichen sclerosus—sensitivity and comfort often improve. Evidence‑based guidelines specifically support therapies such as vaginal estrogen, vaginal DHEA, and ospemifene for genitourinary syndrome of menopause (GSM).
What is clitoral atrophy?
Clitoral atrophy describes reduced responsiveness—and sometimes visible shrinkage—of the clitoral glans (the external tip) and surrounding tissues. It can occur with hormonal changes (e.g., menopause or temporarily during breastfeeding), lower blood flow, or skin conditions that make the glans less accessible. Consumer health references and medical overviews describe clitoral atrophy as decreased response to stimulation, often tied to hypoestrogenism and diminished blood flow.
A quick anatomy refresher helps: the clitoris is a larger, internal erectile organ—not just a “button.” It includes the glans, body, crura, and bulbs, with most of its structure tucked inside and anchored to the pelvis. That’s why your clitoris doesn’t “fall off,” and why changes you notice are usually about surface tissue health or access to the glans rather than a missing organ.
Is clitoral atrophy permanent?
- Low estrogen (GSM) causes thinning, dryness, irritation, and decreased elasticity. Local vaginal estrogen, vaginal DHEA, and ospemifene can thicken tissues, boost lubrication, and reduce pain—often with meaningful symptom relief.
- Postpartum/lactation: temporary low estrogen during breastfeeding can mimic GSM. Emerging literature calls this “genitourinary syndrome of lactation.” Symptoms generally improve as hormones normalize; a clinician may suggest moisturizers/lubricants and, for some, carefully considered local therapy.
- Clitoral hood adhesions (phimosis) & lichen sclerosus (LS): these can hide the glans and reduce sensation. Early treatment—commonly ultra‑potent topical steroids for LS, and conservative management of adhesions—often restores comfort and access; procedural release is reserved for select cases.
- Vascular/nerve factors, medications, and lifestyle: SSRIs/SNRIs, combined hormonal effects, diabetes, smoking, and pelvic surgery can influence arousal or sensation; addressing root causes and gentle, regular stimulation (solo or partnered) can help with responsiveness over time.
Bottom line: For most, clit atrophy is treatable rather than permanent—especially if you tackle the underlying driver early.
Clitoral atrophy symptoms (what to watch for)
If you’re scanning for clitoral atrophy symptoms, you might notice:
- Lower sensitivity or “numb” feeling during stimulation
- Dryness, stinging, or burning with touch or penetration
- A smaller‑looking or “hidden” glans beneath the hood
- Pain with sex (dyspareunia), and sometimes urinary urgency or recurrent UTIs when GSM is present.
Red flags—see a clinician promptly: white, shiny patches; tearing; intense itch or pain (possible lichen sclerosus), new bleeding, or lesions that don’t heal. Early LS treatment prevents scarring.
Why does clitoral atrophy happen? (Main causes)
1) Low estrogen (menopause, surgical menopause, postpartum/lactation)
Estrogen maintains the thickness, elasticity, and lubrication of vulvovaginal tissues. When it drops, tissues thin and become drier and more sensitive to friction, and the glans may seem smaller. GSM guidelines recommend vaginal estrogen, vaginal DHEA, and ospemifene for moderate–severe symptoms, alongside moisturizers and lubricants. Postpartum and lactating individuals can experience a temporary, GSM‑like state that improves as estrogen returns.
2) Reduced arousal and blood flow
Regular sexual arousal (solo or with a partner) supports genital blood flow. When stimulation drops off for long stretches, tissues may feel less responsive—not permanent damage, but a change that often improves with gradual re‑introduction of touch or vibration.
3) Skin conditions causing adhesions (especially lichen sclerosus)
LS can lead to clitoral hood adhesions (phimosis), partially covering the glans and diminishing sensation. First‑line treatment is ultra‑potent topical steroids (e.g., clobetasol) prescribed by a specialist; early care is key. Some cases add estrogen therapy or, rarely, procedural release.
4) Medications & medical conditions
Antidepressants (SSRIs/SNRIs), hormonal contraceptives (via changes in free testosterone), diabetes, smoking, pelvic surgery, and some neurologic conditions can affect arousal or nerve response. Working with your clinician to adjust meds when possible and addressing cardiometabolic health can help.
How clinicians evaluate it
A typical visit may include:
- A vulvar and vaginal exam to check for GSM, fissures, LS, or adhesions
- Vaginal pH testing and infection screening as needed
- A discussion of hormone status, medications, sexual history, and any pelvic surgeries
-
Sometimes dermatology referral or a small biopsy if LS is suspected
This is usually straightforward—and it’s the fastest path to the right treatment.
Evidence‑based treatments that help (and how they work)
First‑line comfort: lubricants & moisturizers
- Water‑based or silicone lubricants for any sexual activity reduce friction and stinging.
- Vaginal moisturizers (non‑hormonal) used several times weekly help restore hydration between encounters. These are standard GSM comfort strategies.
Local hormone options (for GSM)
- Low‑dose vaginal estrogen (creams, tablets, ring): improves tissue thickness, elasticity, and lubrication; low systemic absorption for most users.
- Vaginal DHEA (prasterone): a local precursor that cells convert to estrogens/androgens in the vaginal tissue; improves dryness and dyspareunia.
- Ospemifene (oral SERM): helpful for dyspareunia in postmenopausal patients, including some with estrogen‑dependent cancer histories (individual risk/benefit discussion required).
Treating LS and adhesions
- Lichen sclerosus: ultra‑potent topical steroids (e.g., clobetasol) are first‑line and can prevent scarring.
- Clitoral hood adhesions: often improve when LS is treated; cautious in‑office release is reserved for select cases by experienced clinicians. Do not attempt DIY separation.
Gentle stimulation to restore blood flow
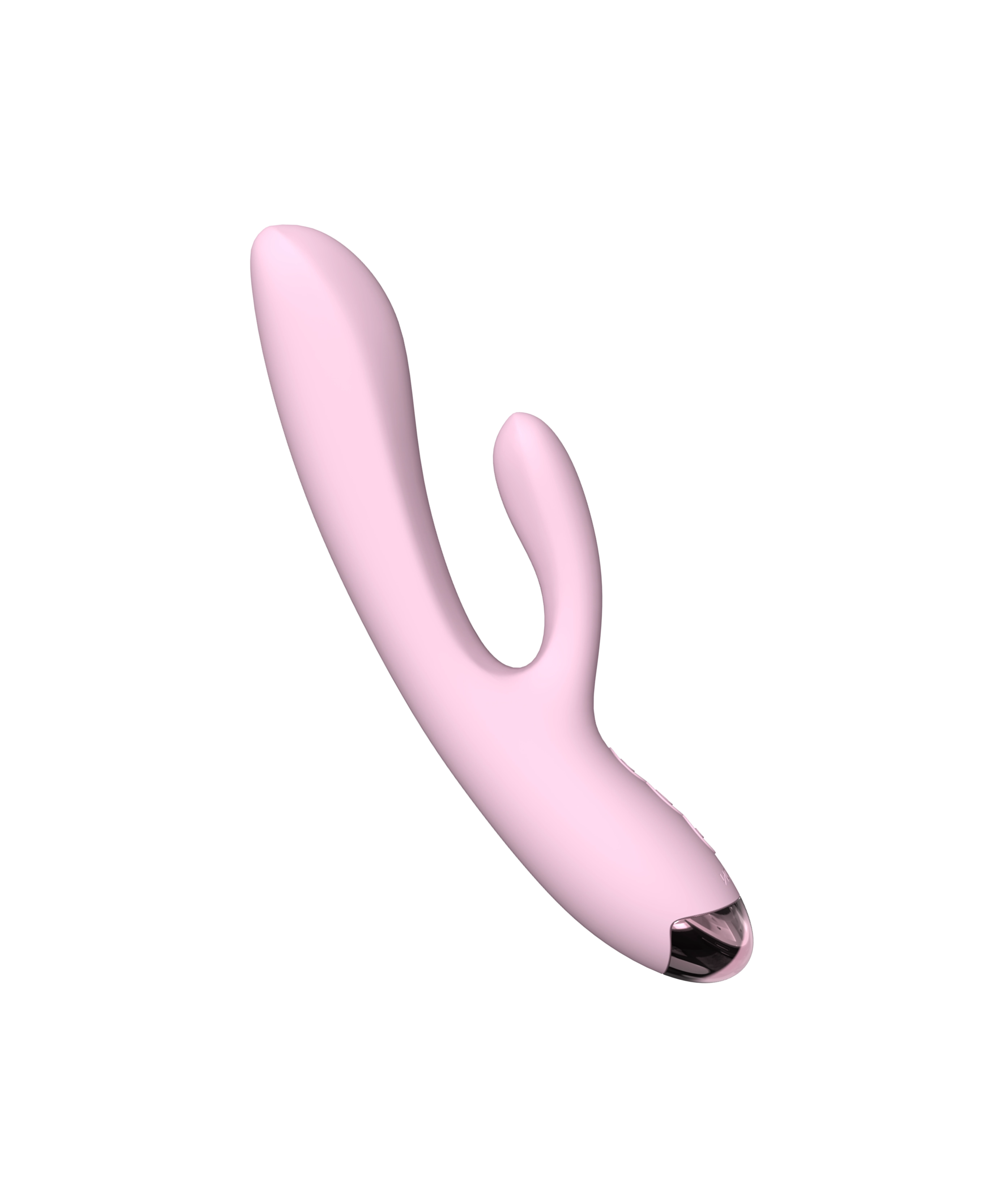
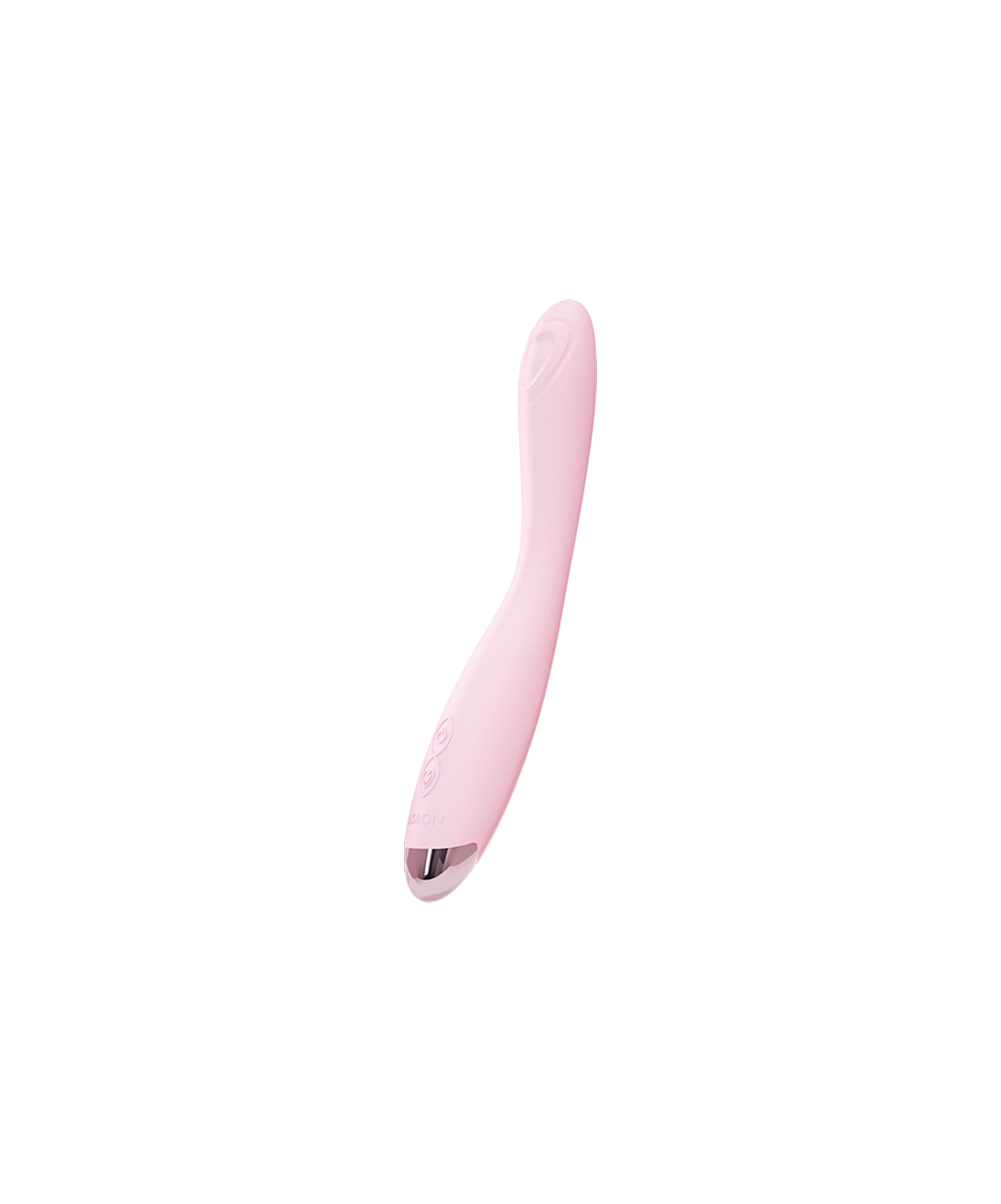
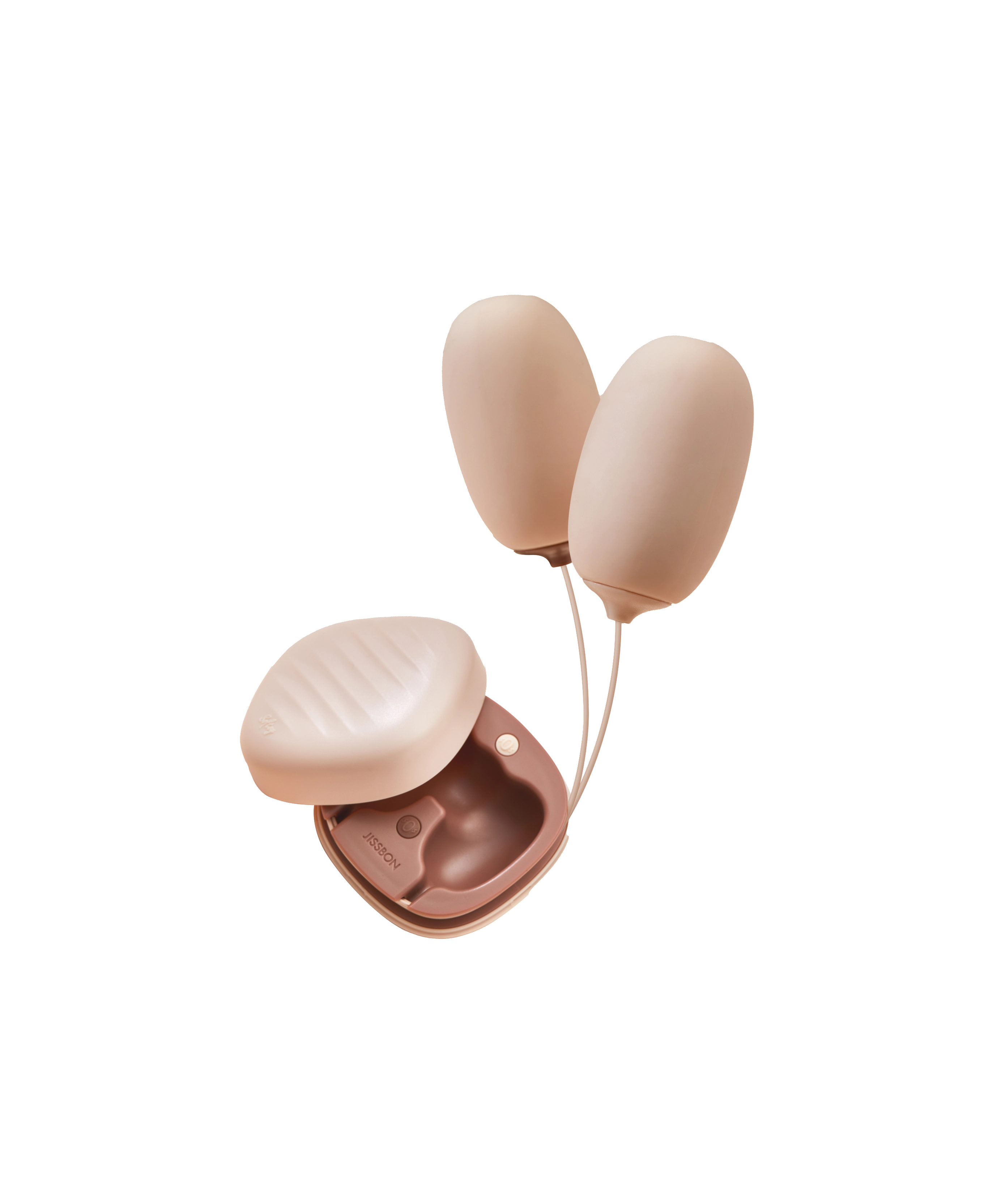
Vibrators are widely used wellness tools; professional sexual‑medicine groups note associations with improved arousal, satisfaction, and pelvic floor function. Used on low settings a few minutes at a time, they can help re‑introduce sensation without friction.
Prefer a soft, targeted device? Explore Clitoral Vibrators or try a gentle suction style like Miss Jelly Clitoral Suction Vibrator to encourage blood flow with minimal rubbing.
A note on energy‑based “rejuvenation”
Laser/radiofrequency “vaginal rejuvenation” devices are not FDA‑approved for GSM and have documented risks (burns, scarring). Major reviews highlight the 2018 FDA safety communication and urge caution. Consider guideline‑supported options first.
A gentle at‑home routine (to support recovery)

Goal: reduce friction, increase blood flow, and work with (not against) healing tissues.
- Moisturize regularly: Apply a vaginal moisturizer 3–5 nights/week; use a neutral emollient externally for comfort.
- Warm‑up matters: Warm compress over underwear for 5 minutes, then light touch around the labia/hood (no pressing if sore).
- Low‑intensity vibration: 3–10 minutes, 3–4 days/week around the clitoral hood or outer labia; stop if numb or irritated.
- Generous lube for any play: Especially if tissues feel dry or thin.
- Lifestyle boosters: Quit smoking, manage blood sugar, and consider pelvic floor PT if you also have pelvic pain or tightness (hypertonicity can reduce pleasure).
Prevention & maintenance
- Don’t wait on symptoms: Early dryness or stinging is easier to treat than entrenched pain.
- Keep tissues active: Regular gentle arousal maintains blood flow—solo or partnered.
- Skin checks: If you notice white patches, tearing, or itch, ask about LS early—steroids work best before scarring.
- Choose body‑safe products: Stick to medical‑grade silicone, and use water‑based lube with silicone toys to protect the surface.
Frequently Asked Questions:
Can you recover from clitoral atrophy?
Often, yes. If your symptoms stem from GSM, local therapies (vaginal estrogen, DHEA, ospemifene) plus moisturizers/lube usually help. If lichen sclerosus or adhesions are involved, steroid treatment and expert care can restore comfort and access. Regular, gentle stimulation supports blood flow and responsiveness.
What does clitoral atrophy look like?
People report a smaller‑looking glans, a glans that seems “hidden” beneath the hood, and drier, more sensitive tissue that stings with touch. When GSM is present, there may be vaginal dryness and pain with sex; when LS is present, you may see white, shiny patches or tearing—get evaluated promptly.
How do you restore clitoral sensation?
Address the cause: re‑hydrate tissues (moisturizers/lube), consider local estrogen, DHEA, or ospemifene for GSM, treat LS if present, and re‑introduce gentle stimulation (e.g., a soft clitoral vibrator on low). Many people see meaningful improvement over weeks to months.
How to fix clitoral nerve damage?
“Nerve damage” covers many scenarios—surgery, childbirth, diabetes, pelvic pain disorders—so recovery depends on the underlying cause. A clinician may suggest pelvic floor therapy, medication changes, or a structured desensitization‑to‑resensitization plan that includes gentle vibration. Seek individualized care if you suspect neuropathy.
What is clitoral atrophy (in simple terms)?
It’s when the clitoral glans becomes less responsive, sometimes smaller‑appearing or harder to access, often due to low estrogen, reduced blood flow, or adhesions. The clitoris itself is internal and anchored—it doesn’t “fall off.” With targeted care, function commonly improves.
The takeaway
If you’ve been worrying “is clitoral atrophy permanent?”, take heart: in most cases, no. What you’re noticing is typically reversible with the right approach—comfort care (moisturizers/lube), guideline‑supported local therapies for GSM, early treatment of LS/adhesions, and gentle re‑stimulation of blood flow. Avoid unproven “rejuvenation” procedures and lean on treatments with real data behind them. Your comfort and pleasure matter—and they’re usually recoverable.
Read more

If you’re shopping your first toy (or upgrading an old favorite), you’ve probably asked: what’s the difference between a dildo and a vibrator? In simple terms, a dildo is typically a non‑motorized ...

If you’ve ever wished solo time felt less rushed and more meaningful, this tantric masturbation guide is for you. Rather than “getting off” as fast as possible, tantric masturbation invites slow, m...