Clitorodynia, clitoral pain that can burn, sting, throb, or feel raw—has many possible causes, from skin irritation to nerve issues. In medical language, clitorodynia is considered a localized subtype of vulvodynia (persistent vulvar pain), which means it may be triggered by a condition (like lichen sclerosus or infection) or be “idiopathic” (no single clear cause). The good news: most causes are treatable with a mix of gentle self‑care and targeted therapies.
Quick answer: how do you get clitorodynia?
- Irritants and friction: fragranced soaps, tight clothing, daily liners, lingering sweat/urine, hair‑removal irritation, or over‑vigorous stimulation can inflame delicate clitoral skin.
- Skin conditions: lichen sclerosus, eczema, psoriasis and contact dermatitis may cause pain, burning, or tearing around the clitoris.
- Hormonal shifts: low estrogen states (menopause, surgical menopause; also postpartum/lactation) can thin and dry tissues, making them sore.
- Infections: yeast, herpes and others can cause clitoral pain or sensitivity.
- Neuropathic causes: pudendal or dorsal clitoral nerve irritation/entrapment (e.g., after surgery, trauma, prolonged cycling, or rarely medical procedures) may trigger burning or electric pain.
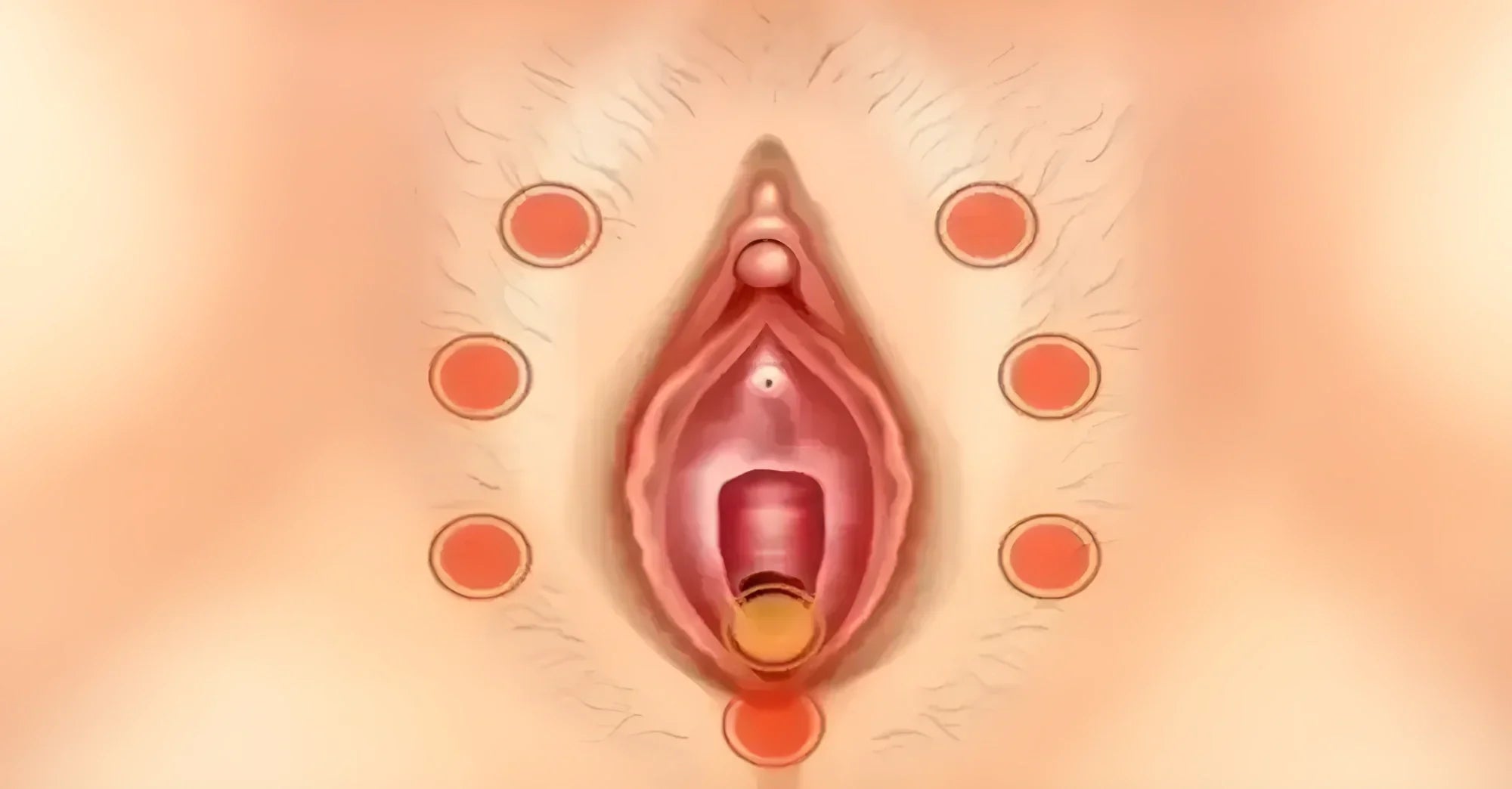
- Structural changes: clitoral hood adhesions/phimosis (sometimes from lichen sclerosus) can trap debris and create tender “keratin pearls.” These can be painful until treated.
If you’re thinking “why does my clit hurt?” it helps to know that clinicians sort clitoral pain the same way they sort other vulvar pain—by location, triggers and duration—to pinpoint the best treatment.
Clitorodynia vs. vulvodynia: how they’re related

By current consensus, vulvodynia is vulvar pain lasting ≥3 months without a clearly identifiable cause; it’s then described as generalized or localized. Clitorodynia is localized pain focused at the clitoris. A cotton‑swab (“Q‑tip”) test and careful exam help map painful spots and distinguish localized from generalized pain.
Symptoms: what clitorodynia can feel like
- Burning, stinging, throbbing, or raw soreness on or under the clitoral hood
- Pain that’s provoked by touch/pressure (sex, tight clothes, wiping) or spontaneous
- Hypersensitivity to vibration or direct pressure; soreness after intense stimulation
- Sometimes visible skin changes if a dermatologic condition (e.g., lichen sclerosus) is present—white, shiny patches, tearing, or scarring/“buried” glans under the hood (these are red‑flag signs—see a clinician).
The most common causes, explained

Irritants & friction
Why it happens: The clitoral glans and hood are exquisitely innervated. Friction (from tight clothing, thongs, rough sex, or even certain bike seats) and chemical irritants (perfumed washes, deodorant pads, scented wipes) can trigger inflammation and pain. Vulvar care handouts consistently recommend fragrance‑free routines, cotton underwear, and avoiding tight garments.
Relief basics: stop irritants, switch to water‑only cleansing, and choose breathable fabrics. If you cycle, consider a pressure‑relieving saddle and limit time seated continuously.
Skin conditions (dermatologic)
Lichen sclerosus (LS) can thin the skin, cause fissures, and create hood adhesions that trap debris and hurt. High‑potency topical steroids are first‑line and prevent scarring; some cases need procedural release of adhesions. Psoriasis and eczema can also affect the vulva and respond to tailored topical therapy and trigger avoidance.
Hormonal changes
Low estrogen (menopause; surgical menopause; sometimes postpartum/lactation) leads to dryness and tissue fragility, which can make the clitoris painful. Treatments for genitourinary syndrome of menopause (GSM) include vaginal estrogen, DHEA, and other options—discuss risks/benefits with your clinician.
Infections
Yeast or HSV outbreaks can cause clitoral pain and burning. Because treatments differ, clinicians may swab, culture, or examine lesions to verify the cause.
Neuropathic pain
Irritation or entrapment of the pudendal nerve or its dorsal clitoral branch can create sharp, burning, or shock‑like pain, often worse with sitting and sometimes following surgery, trauma, or prolonged cycling. Diagnosis may include nerve blocks, imaging, and pelvic floor assessment; treatments range from pelvic floor physical therapy to nerve blocks and selected medications for neuropathic pain.
Structural issues: clitoral hood adhesions & keratin pearls
With lichen sclerosus or chronic inflammation, the hood can partially fuse over the glans (clitoral phimosis). Trapped debris (“keratin pearls”) under the hood can be exquisitely tender. Specialists may use topical therapy to calm inflammation and perform in‑office lysis if needed.
How doctors diagnose clitorodynia
Expect a gentle vulvar exam, a Q‑tip pain map, review of products/clothing/activities, and—if indicated—tests to rule out infections or dermatologic disease (occasionally biopsy for LS). Many guidelines recommend evaluating for pelvic floor dysfunction because hypertonic muscles can magnify pain. Diagnosis is individualized and sometimes requires a multidisciplinary team (gynecology, dermatology, pelvic floor PT, pain specialist).
Clitorodynia treatment at home: gentle, science‑backed habits

These are comfort measures—not a substitute for diagnosis. Use them while you seek care or alongside medical treatment.
- Strip out irritants. Use water only on the vulva; skip douches, perfumes, scented wipes, and daily liners. Switch to fragrance‑free detergent; wear 100% cotton underwear; avoid tight pants and pantyhose.
- Moisture & barrier. If skin is dry or chafed, a thin film of plain petrolatum (over intact skin) can lock in moisture and reduce friction.
- Cool or lukewarm soaks. Sitz baths (cool‑to‑lukewarm) may calm burning and help you relax pelvic muscles.
- Smart lube. For any touch or sex, use a generous water‑based lubricant; reapply often. (If using latex condoms, avoid oil‑based products.)
- Pelvic floor down‑training. Slow belly breathing (e.g., inhale 4, exhale 6) and gentle relaxation can reduce guarding and sensitivity; PT can teach this in more detail.
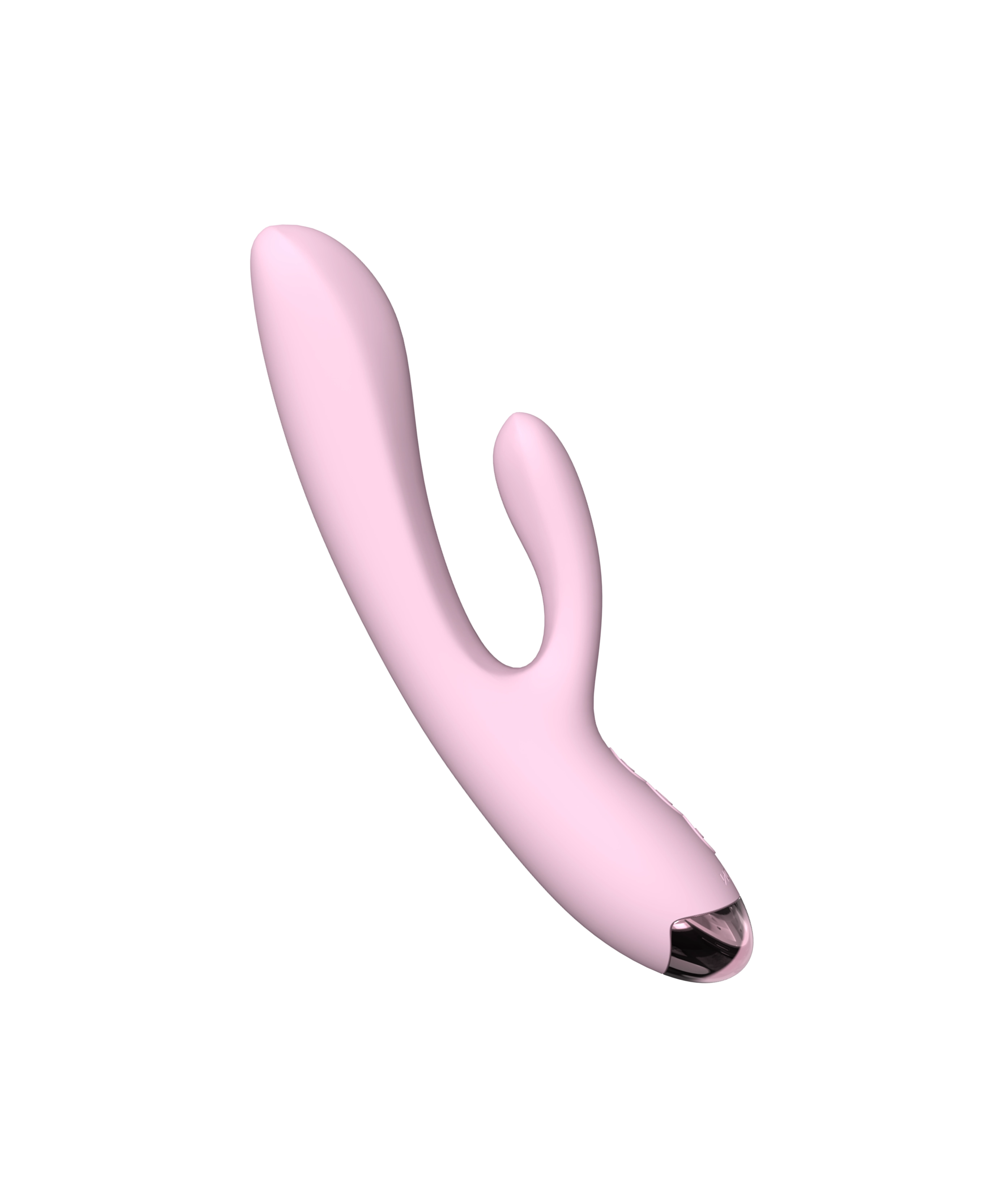
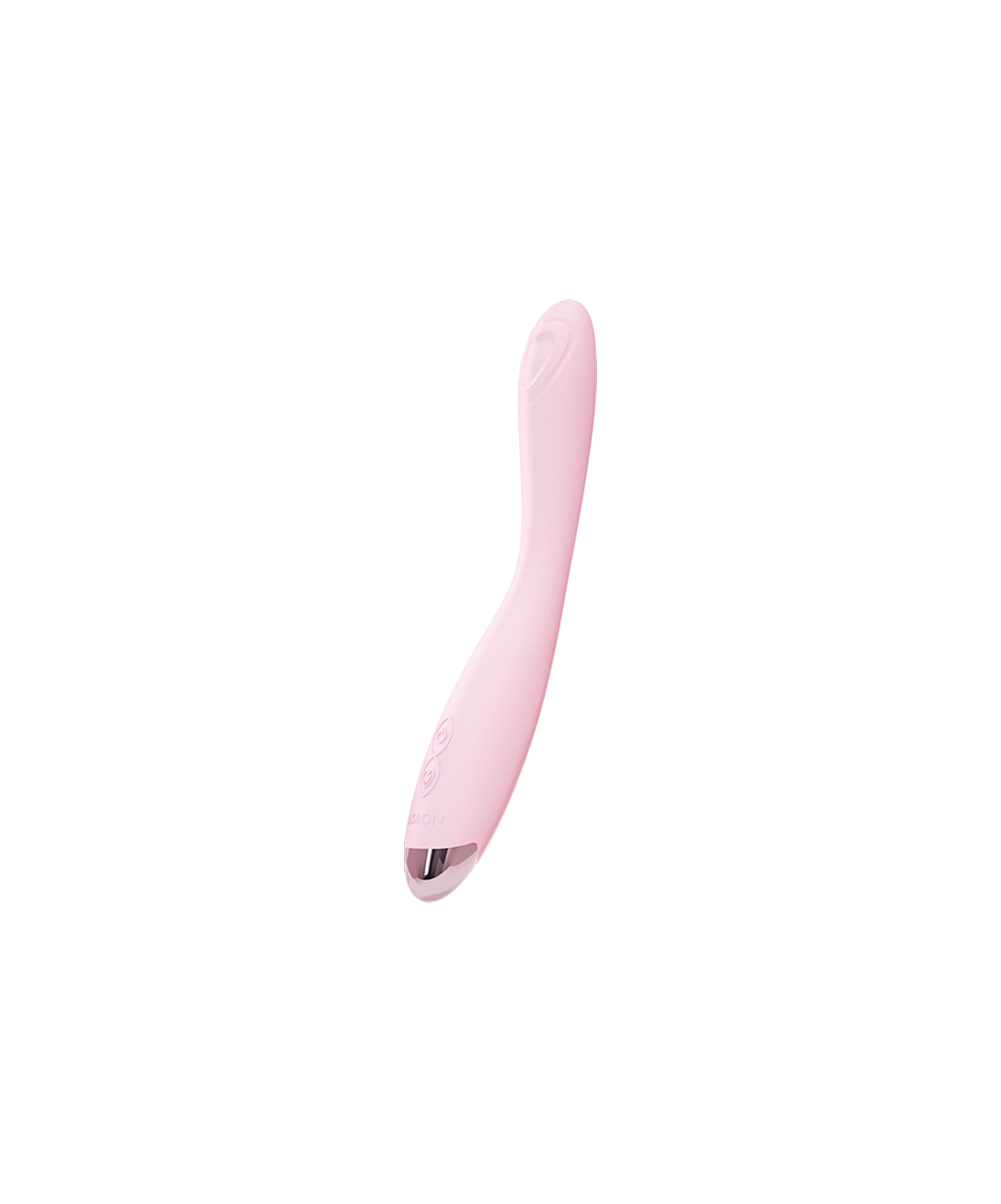
- Go easy with devices. If vibration or direct pressure increases soreness, pause; when you’re ready to reintroduce sensation, start with broad, low‑intensity external touch. (Direct, high‑intensity pressure can cause temporary soreness in some people.) Explore gentle options in Sex Toys for Women only after symptoms settle.
A note on numbing creams: many vulvar pain resources caution that topical anesthetics often provide limited relief and can irritate; discuss with your clinician before use.
Medical treatments that help (tailored to the cause)
Treat the specific condition (if present)
- Lichen sclerosus: high‑potency topical steroids are gold standard and reduce scarring/adhesions; refractory adhesions may be released by an experienced clinician.
- Infections: targeted antifungals/antivirals/antibiotics, depending on diagnosis.
- Hormonal deficiency (GSM): vaginal estrogen, DHEA or other options may restore tissue comfort; your clinician will weigh benefits/risks.
Address pelvic floor & nerve contributors
- Pelvic floor physical therapy/biofeedback: first‑line for many with vulvar pain, especially if muscles are tight/guarded.
- Neuropathic pain strategies: for pudendal or dorsal clitoral neuralgia, options include nerve blocks, selected medications (e.g., tricyclics, anticonvulsants/SNRIs), and in select cases targeted nerve procedures—all individualized by a specialist.
Structural care for clitoral hood adhesions/“keratin pearls”
-
Topical therapy for inflammation (often steroids when LS is present) plus gentle in‑office lysis can free the hood and remove painful debris; a few cases require surgical correction.
Treatment plans for vulvar pain are typically multidisciplinary and stepped; no single therapy works for everyone, and progress is often gradual—but meaningful.
Prevention & flare management
- Minimize friction: breathable fabrics; change out of sweaty clothing; use lube for any genital touch.
- Mind the saddle: if you bike, use a cutout/pressure‑relief seat and adjust posture/fit; take breaks. (Prolonged pressure can irritate pelvic nerves.)
-
Hair removal hygiene: if you remove hair, avoid dry shaving; use clean tools and soothing, unscented emollients afterward.
- Gentle sexual pacing: avoid prolonged high‑intensity stimulation; take breaks and vary pressure. If you notice post‑play soreness, rest a day or two and return more gently.
When to seek care—sooner, not later
See a clinician if you notice white, shiny patches; tearing; bleeding; new lesions; fever; foul discharge; or pain that persists beyond two weeks despite irritant‑avoidance. These can indicate conditions like lichen sclerosus, infection, or other disorders that benefit from early treatment.
Ready to re‑introduce pleasure—gently?
Once pain settles and your clinician gives the okay, some people find gradual, broad external stimulation helpful to rebuild comfort and blood flow. Keep settings low and brief, use plenty of lube, and stop if anything burns or stings. If you’re exploring gentle tools, browse Sex Toys for Women and look for soft silicone, rounded edges, and low‑intensity modes.
Bottom line
If you’re asking “how do you get clitorodynia?”, the answer is usually a mix of factors—skin, hormones, nerves, friction, and sometimes adhesions. The path forward is systematic but hopeful: remove irritants, use comfort strategies, and partner with a clinician to treat specific conditions (e.g., topical steroids for LS, vaginal estrogen for GSM, pelvic floor PT, or nerve‑focused care when needed). With time and tailored treatment, clitoral pain can improve, and your relationship with pleasure can, too.
Frequently Asked Questions:
Does clitorodynia go away?
Often, yes—especially when the root causes (irritants, infections, hormonal changes, adhesions, pelvic floor tension, or nerve irritation) are identified and treated. Many people improve with vulvar care, pelvic floor PT, and cause‑specific therapies like topical steroids for LS or vaginal estrogen for GSM. Recovery is typically gradual and individualized.
How did I get clitorodynia?
Common pathways include friction/irritants, skin disease (e.g., lichen sclerosus), hormonal thinning, infections, nerve‑related pain (pudendal or dorsal clitoral nerve), and clitoral hood adhesions that trap debris. A clinician can help sort overlapping factors and build a plan.
Why is my clitoral hood irritated?
Often contact dermatitis, friction, or LS; sometimes debris under a partially fused hood (adhesions) causes tender “keratin pearls.” Remove irritants, use water‑only cleansing, and seek evaluation—especially if you see white patches or tearing.
Does clitorodynia mean I have an STI or cancer?
Not usually. Infections and (rarely) neoplasia are on the differential, which is why clinicians examine the area and test when needed. Getting checked is the fastest path to appropriate treatment and peace of mind.
What clitorodynia treatment at home is safe to try first?
Start with irritant‑avoidance, cool/lukewarm sitz baths, plain petrolatum as a barrier on intact skin, ample water‑based lube, and gentle pelvic floor relaxation. If pain persists or you notice red‑flag skin changes, book an appointment.
Read more

If you’re comparing a glass vs silicone dildo, you’re already asking the right question. Material shapes everything—from the feel and pressure to temperature play, lubricant compatibility, cleaning...

If you’ve ever wondered “can you desensitize your clitoris?”—especially after a strong vibrator session—you’re not alone. Many people worry about a desensitized clitoris, ask whether vibrators decr...