Clitoris atrophy is the shrinking and loss of function of the clitoris, often linked to aging, menopause, or hormonal changes. It can affect sexual pleasure and sensitivity, and may be accompanied by other urogenital symptoms.
Understanding clitoral atrophy, its causes, and prevention methods can help maintain sexual wellness and comfort. In this guide, we’ll cover the key symptoms, practical ways to support clitoral health, and tools that can help, including body-safe sexual wellness products.
Who Experiences Clitoral Atrophy & Quick Benefits of Awareness
Clitoral atrophy can occur in a variety of scenarios, and awareness is the first step toward maintaining sexual health:
- Menopause & aging: Hormonal drops reduce blood flow and tissue elasticity.
- Post-pregnancy or extended inactivity: Less stimulation can lead to tissue thinning.
- Medication use: Certain antidepressants, hormone therapies, or cancer treatments may contribute.
- Medical conditions: Lichen sclerosus and other genital skin conditions may affect clitoral tissue.
Benefits of understanding clitoral atrophy:
- Early recognition of symptoms like reduced sensitivity or size
- Knowledge of prevention through stimulation and hormone support
- Better sexual satisfaction and comfort
How to Support Clitoral Health

While medical consultation is essential, practical lifestyle and wellness habits can help maintain clitoral function:
- Regular stimulation: Masturbation or sexual activity increases blood flow.
- Moisturizers & lubricants: Use water-based vaginal moisturizers to maintain tissue elasticity.
- Hormone therapy (if advised): Estrogen creams or testosterone treatments may be recommended.
- Exercise: Cardio improves overall circulation, including genital blood flow.
- Avoid irritants: Scented products or harsh cleansers can worsen sensitivity.
External resources for guidance include Cleveland Clinic’s tips on reducing irritation safely and what the clitoris is for anatomical context.
Clitoral Atrophy vs Alternatives: Understanding the Options
Some may explore sexual wellness tools to enhance clitoral stimulation and improve blood flow. Here’s a quick guide to options:
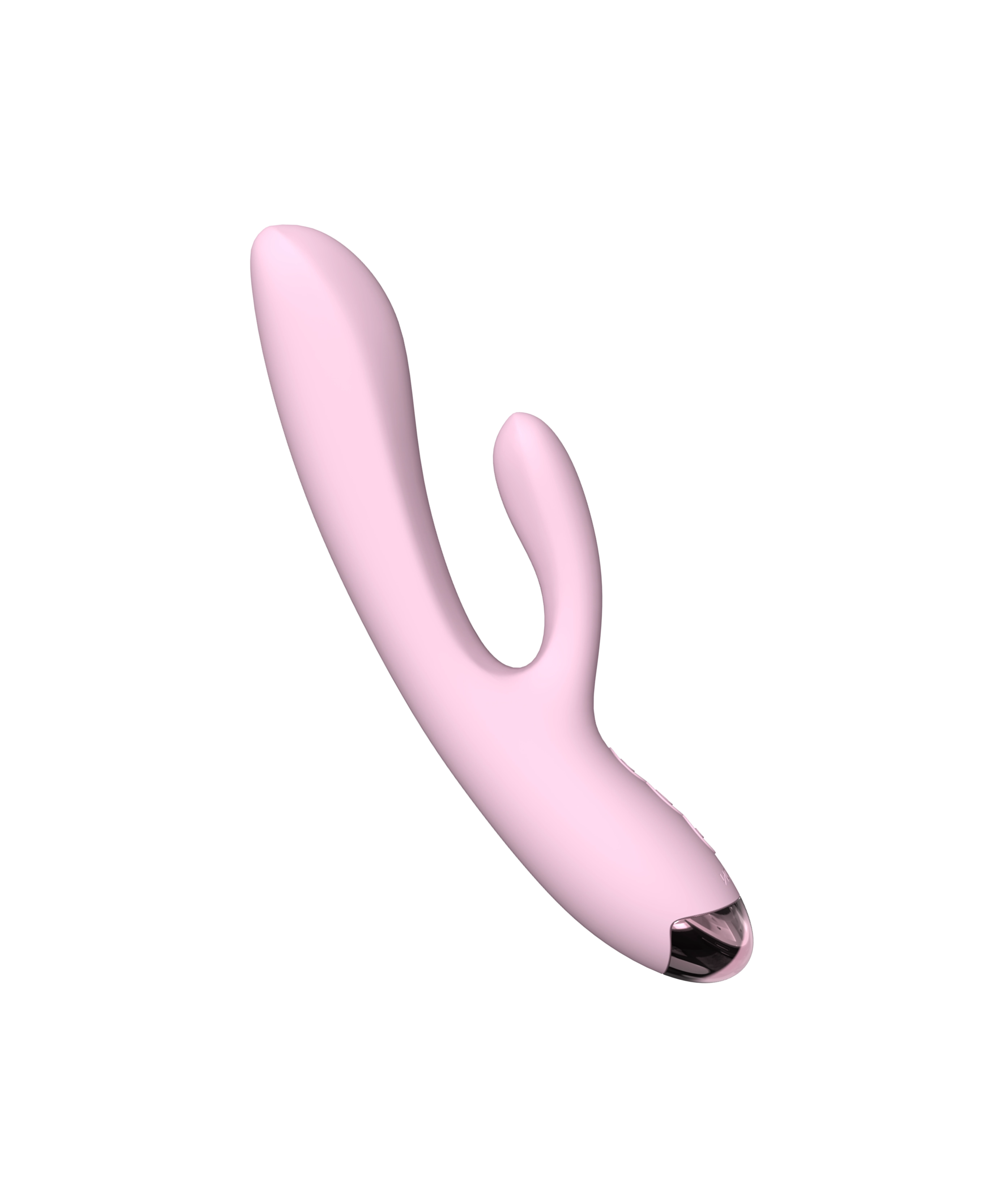
- Rabbit vibrators: Target G-spot and clitoral stimulation simultaneously; best for dual sensations.
- Wand vibrators: Powerful, broad stimulation for desensitized or atrophied tissue.
- Bullet vibrators: Focused, precise stimulation; ideal for beginners or sensitive skin.
- G-spot stimulators: Indirect clitoral stimulation through internal arousal.
- Prostate massagers (for partners): Enhance mutual pleasure and overall sexual satisfaction.
For targeted clitoral care, consider a remote controlled bullet vibrator like the Invisible Pink Remote Controlled Bullet Vibrator for personalized control and comfort.
Step-by-Step Guide to Gentle Use
- Prep: Wash the toy with mild soap or a toy cleaner, charge fully, and patch-test lubricants.
- Start slow: Begin with low intensity to gauge sensitivity.
- Explore angles & pressure: Light circular or pulsating motions work best.
- Take breaks: Check comfort regularly to avoid irritation.
Lube & Compatibility 101
- Water-based lubricants: Safe with silicone toys, gentle on sensitive tissue.
- Silicone-based lubricants: Provide longer-lasting glide but may degrade silicone toys.
- Condom use: Ensure compatibility when sharing toys.
- Moisturizer tips: Avoid scented or chemical-laden products to reduce irritation.
Care & Maintenance
- Before & after use: Rinse with warm water and mild soap or toy cleaner.
- Drying & storage: Air-dry or towel-dry; store in a clean, dry pouch.
- Charging safety: Only use approved chargers; avoid water exposure.
- Material-specific care: Silicone, ABS, or TPE have different cleaning needs; follow manufacturer guidelines.
Advanced Strategies to Support Clitoral Health
For individuals experiencing or concerned about clitoral atrophy, combining lifestyle, sexual wellness, and medical strategies can maximize comfort and pleasure.
Hormonal Support Options
- Local estrogen therapy: Creams, tablets, or rings can target clitoral and vaginal tissue directly, helping restore elasticity.
- Systemic hormone therapy: Sometimes recommended for overall menopausal symptom relief, but should be supervised by a doctor.
- Testosterone therapy: Low-dose therapy may be advised in select cases to improve clitoral sensitivity; professional guidance is essential.
- Always discuss options with a gynecologist or endocrinologist to balance benefits and risks.
Role of Sexual Wellness Tools
Sexual stimulation can significantly improve blood flow and tissue health. Tools can be chosen based on comfort, sensitivity, and desired stimulation type.
Popular Options
- Clitoral vibrators: Focused stimulation helps maintain nerve function and pleasure; suitable for both beginners and experienced users.
- Suction stimulators: Offer gentle pulsing sensations that can improve circulation without excessive friction.
- Wand vibrators: Broader stimulation for desensitized tissue or multi-area use.
Compare & Decide:
|
Tool Type |
Best For |
Notes |
|
Bullet Vibrators |
Precision & sensitive skin |
Small, portable, targeted |
|
Wand Vibrators |
Powerful stimulation |
Can help reverse mild atrophy |
|
Rabbit Vibrators |
Dual stimulation |
Combines G-spot + clitoral stimulation |
|
Suction Devices |
Circulation & nerve activation |
Non-invasive, gentle pulse |
Tip: Rotate tools occasionally to stimulate different nerve pathways and enhance blood flow.
Lifestyle Factors That Influence Clitoral Health
Lifestyle plays a critical role in maintaining clitoral tissue and sexual function.
Exercise & Circulation
- Cardio exercises like walking, swimming, or cycling improve overall blood flow.
- Pelvic floor exercises (Kegels) strengthen muscles supporting the clitoris and vagina.
Nutrition
- Diets rich in omega-3s, antioxidants, and phytoestrogens may support hormonal balance.
- Hydration helps maintain tissue elasticity and natural lubrication.
Stress Management
- Chronic stress can reduce sexual desire and affect circulation.
- Mindfulness, yoga, or meditation can help maintain sexual wellness.
Avoid Irritants
- Fragranced soaps, douches, or harsh chemicals can exacerbate atrophy symptoms.
- Use mild, pH-balanced cleansers for genital hygiene.
Prevention Tips for Clitoral Atrophy
Even before symptoms arise, preventative measures can maintain clitoral health and sensitivity.
- Maintain regular sexual activity: Frequency doesn’t have to be high; even gentle stimulation aids blood flow.
- Use appropriate lubrication: Water-based moisturizers prevent dryness and tissue thinning.
- Explore different types of stimulation: Vary intensity, angles, and toy types.
- Routine checkups: Regular gynecological visits help monitor hormonal levels and tissue health.
- Pelvic floor strength: Strengthening muscles improves circulation and sexual satisfaction.
Emotional & Relationship Considerations
Clitoral atrophy can impact self-esteem, sexual confidence, and intimate relationships. Recognizing and addressing emotional aspects is equally important.
- Communication: Discuss changes openly with partners; explore shared solutions like mutual stimulation.
- Counseling: Sex therapists or counselors can provide coping strategies and guidance.
- Mindful pleasure: Focus on overall sensation and intimacy rather than performance.
Exploring Sex Toy Care & Safety in Depth
Using sexual wellness tools safely is critical for maintaining tissue health.
Cleaning & Storage
- Wash toys before and after use with mild soap or toy-specific cleaner.
- For silicone toys, avoid silicone-based lubricants that can degrade the material.
- Store toys in a dry pouch, away from direct sunlight or extreme heat.
Lubricant Guidelines
- Water-based lubricants: Safe for all toys, ideal for sensitive tissue.
- Silicone-based lubricants: Longer-lasting but avoid with silicone toys.
- Hybrid lubricants: Combination formulas can provide extended glide.
Battery & Charging Safety
- Fully charge rechargeable toys before first use.
- Avoid water exposure during charging.
- Replace batteries or rechargeable units as recommended to maintain consistent power and performance.
When to Seek Professional Guidance
While lifestyle and sexual wellness tools help, professional evaluation is essential when:
- You notice persistent reduced clitoral size or loss of sensitivity
- Symptoms include pain, itching, or burning
- Hormonal therapy is being considered
- You experience urinary issues associated with Genitourinary Syndrome of Menopause (GSM)
Frequently Asked Questions
What causes clitoral atrophy?
Clitoral atrophy typically results from reduced estrogen or testosterone levels, aging, lack of stimulation, or certain medications. Conditions like lichen sclerosus can also contribute.
Can clitoral atrophy be reversed?
While some tissue loss may be permanent, stimulation, hormone therapy, and regular sexual activity can improve blood flow, sensitivity, and sexual satisfaction.
Is hormone therapy necessary?
Not always. Many individuals manage symptoms with moisturizers, sexual activity, or targeted stimulation. Consult a healthcare professional for personalized advice.
Which sex toys help with clitoral atrophy?
Body-safe vibrators like bullets, wands, or suction devices can enhance blood flow and pleasure. Explore options like clitoral vibrators for targeted stimulation.
Are there lifestyle habits that prevent atrophy?
Regular exercise, sexual activity, maintaining lubrication, and avoiding irritants can help preserve tissue health.
Conclusion
Clitoral atrophy is a common, manageable aspect of sexual health, especially during aging or hormonal changes.
Awareness, gentle stimulation, and supportive tools like a remote controlled bullet vibrator can help maintain sensitivity and pleasure. Explore more options in our clitoral vibrators collection for body-safe, enjoyable solutions. Visit Jissbon to browse all sexual wellness products.