Short answer: No—your clit can’t “fall off.” The clitoris is not a tiny, detachable button; it’s a complex erectile organ with internal roots (the crura and bulbs) anchored under the pelvic bone. Only a small portion (the glans) is visible externally. That internal structure—and its dense nerve network—doesn’t just fall away.
That said, some people notice that the clitoral tip feels smaller, less sensitive, or “hard to find.” This experience is often tied to clitoral atrophy or conditions that hide the glans (like clitoral hood adhesions) rather than any literal loss of the clitoris. This guide explains what clitoral atrophy is, why it happens, how to spot symptoms, and the most evidence‑based ways to restore comfort and pleasure.
Quick anatomy refresher (for peace of mind)
- Most of the clitoris is internal. The visible glans is the tip of a larger organ ~9–11 cm wide when mapped internally. It’s made of erectile tissue, like the penis, and becomes engorged with arousal.
- Because it’s anchored inside the pelvis, there’s no ordinary scenario where the clitoris detaches or “falls off.” If you’re worried after pain, trauma, or a new lesion, that’s a reason to see a clinician—not a sign of loss.
What is clitoral atrophy?
Clitoral atrophy describes decreased responsiveness and potential shrinkage of the clitoral glans over time, usually due to hormonal changes and/or reduced blood flow to genital tissues. It’s often discussed alongside genitourinary syndrome of menopause (GSM)—the modern medical term for vulvovaginal/urinary changes from low estrogen (dryness, thinning, discomfort, and urinary symptoms).
Common causes (and how they connect to your symptoms)
Estrogen drop (menopause, perimenopause, postpartum & lactation, ovarian surgery)
Low estrogen thins genital tissues, reduces natural lubrication, and raises pH—making friction more irritating and arousal more difficult. This can come with menopause, after removal of the ovaries, or while breastfeeding (temporary “lactational hypoestrogenism”).
-
Postpartum & breastfeeding: It’s normal to have dryness and pain from lower estrogen; some studies show localized estrogen can help select postpartum patients. Talk to your clinician if symptoms persist—especially while nursing.
Decreased blood flow and arousal (“disuse”)
Regular arousal—solo or partnered—supports genital blood flow. People who stay sexually active often report milder atrophic symptoms than those who stop. This doesn’t mean you must have intercourse; gentle stimulation counts.
Clitoral hood adhesions & lichen sclerosus (LS)
Sometimes, scar‑like adhesions form between the hood and the glans (clitoral phimosis). The glans can seem “buried,” and sensitivity drops. Lichen sclerosus—a chronic inflammatory skin condition of the vulva—is a frequent cause and is treatable, typically with high‑potency topical steroids (e.g., clobetasol) prescribed by a specialist. Early treatment helps prevent scarring.
-
Labial or hood adhesions can also occur in very low‑estrogen states and may respond to estrogen cream or careful separation by a clinician when needed.
4) Medications & health conditions
- Antidepressants (SSRIs/SNRIs) can blunt libido, arousal, orgasm, and genital sensation in some users (sometimes even after discontinuation). This is not “atrophy,” but it can feel similar. Work with your prescriber if this matches your timeline.
- Hormonal contraceptives may lower free testosterone (mixed effects on desire overall). This can influence arousal and lubrication—again, not true atrophy, but relevant to sensation.
- Diabetes, smoking, vascular issues also affect blood flow and nerve function. Addressing these can improve sexual comfort.
Clitoral atrophy symptoms (what you might notice)
- Decreased sensitivity or “numbness” during stimulation
- Dryness, burning, or stinging with touch or penetration
- The clitoral tip looks smaller or “hidden” under the hood
- Painful sex (dyspareunia), urinary urgency or recurrent UTIs (often tied to GSM)
If you also see white, shiny patches; tearing; or intense itching, ask about lichen sclerosus—a treatable skin condition that can cause adhesions and scarring if ignored.
Can clitoral atrophy be reversed?
Often, yes—improvement is common with the right plan. Think of it as restoring hormones + hydration + healthy blood flow and treating any skin condition that’s in the way.
Rehydrate tissues: lubricants & moisturizers
- Use a generous, body‑safe lubricant any time you touch or play.
- Add a vaginal moisturizer several times per week (look for hyaluronic‑acid or polycarbophil bases if you prefer non‑hormonal support).
Restore estrogen locally (if appropriate)
For GSM symptoms, leading guidelines support low‑dose vaginal estrogen (creams, tablets, or an estrogen ring), vaginal DHEA, or ospemifene (an oral SERM). These options thicken tissue, improve lubrication, and often reduce pain. Discuss risks and benefits with your clinician—especially if you have a history of estrogen‑sensitive cancer.
Encourage healthy blood flow
- Gentle, regular arousal helps—solo or partnered.
- Many clinicians consider vibrators a helpful wellness tool: studies and professional groups report associations with increased arousal, lubrication, and orgasmic function (and possibly pelvic floor benefits).
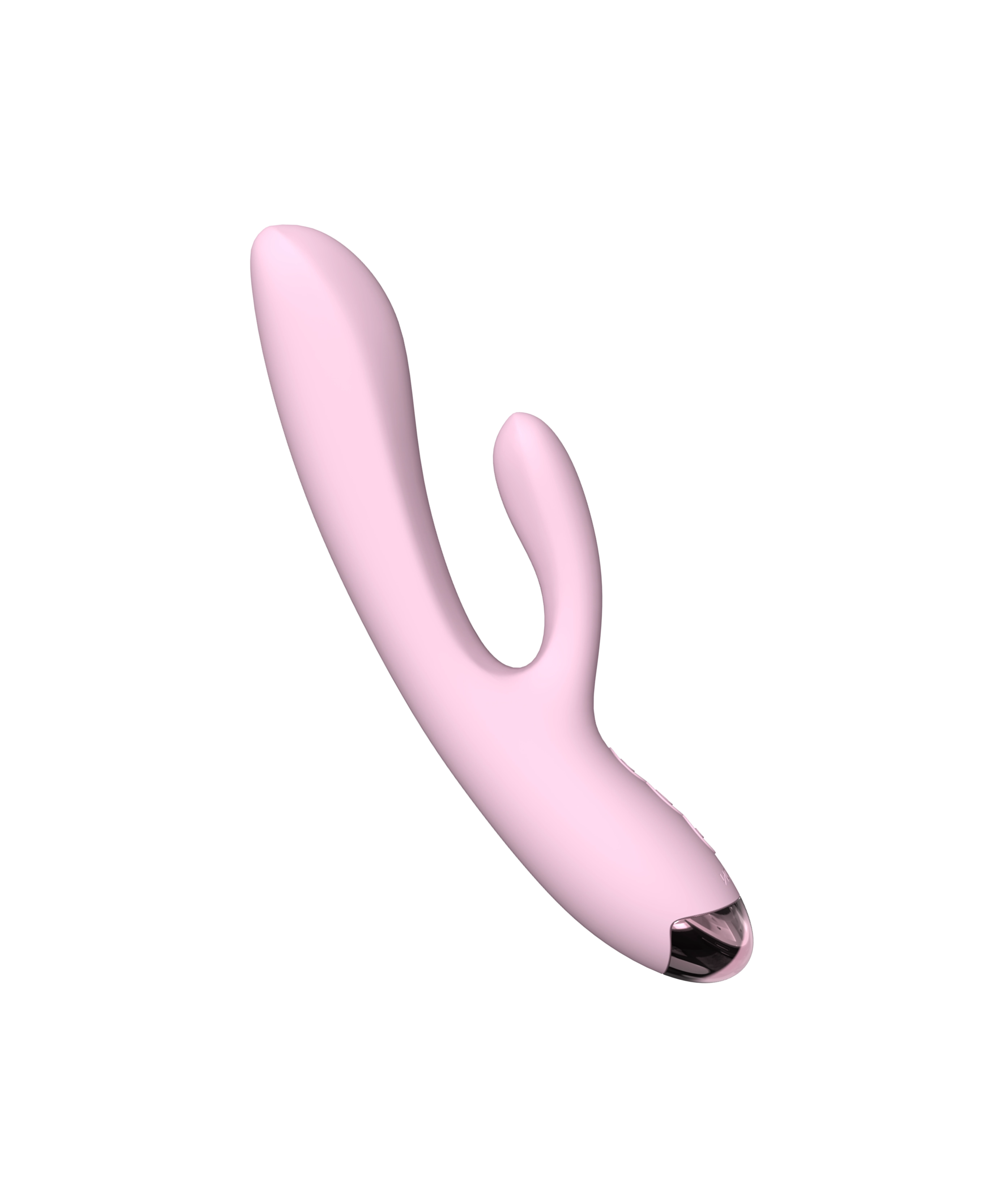
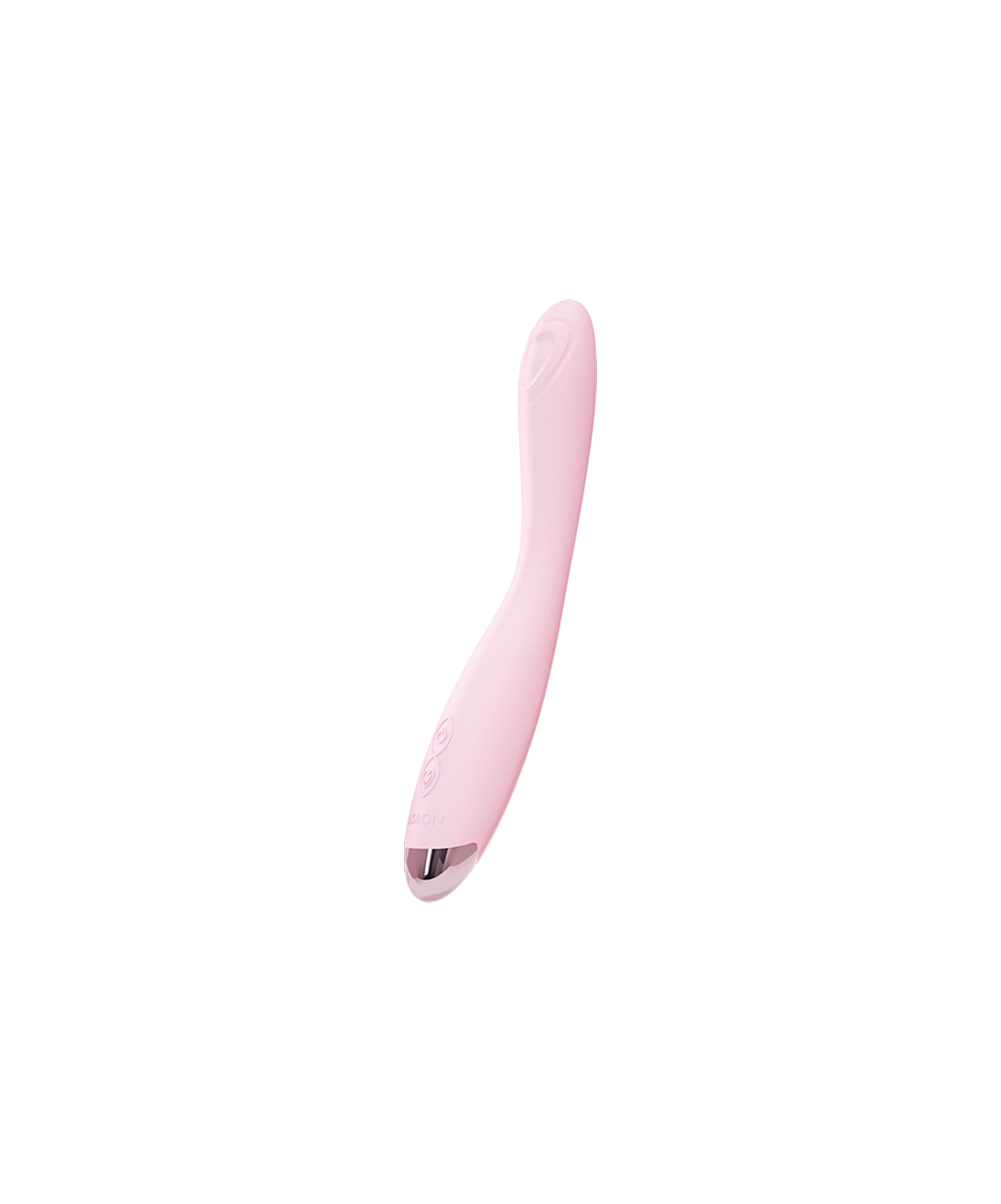
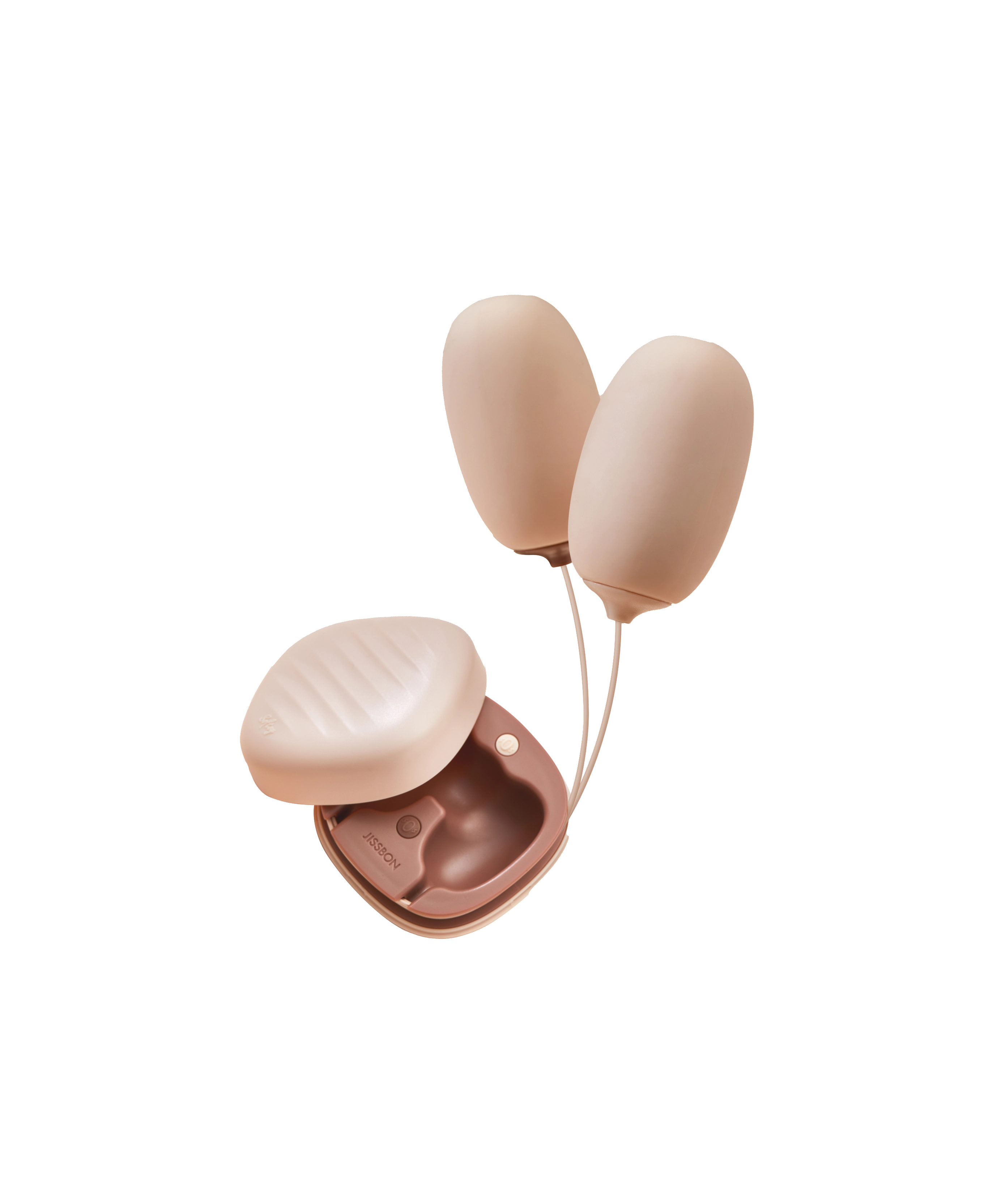
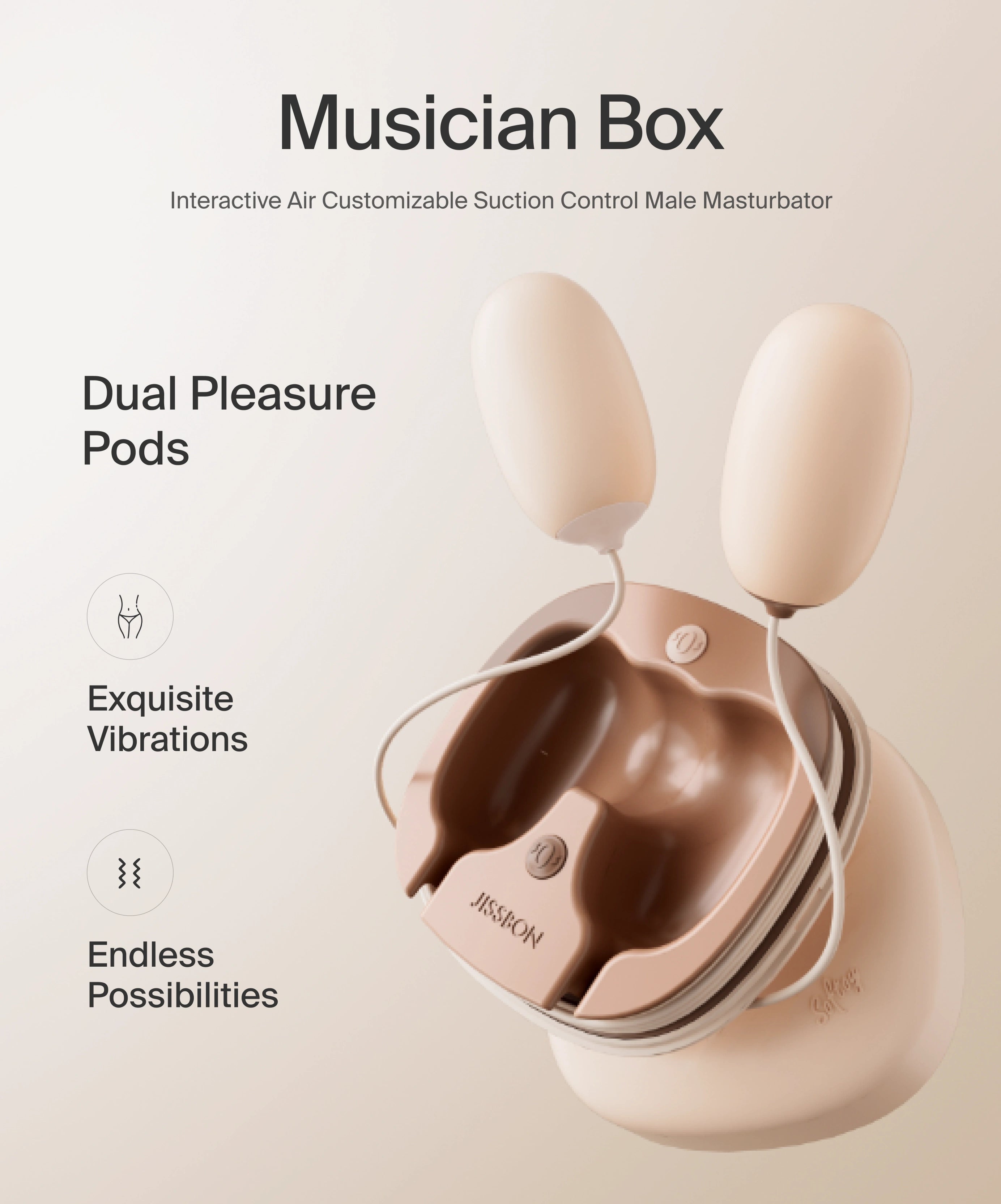
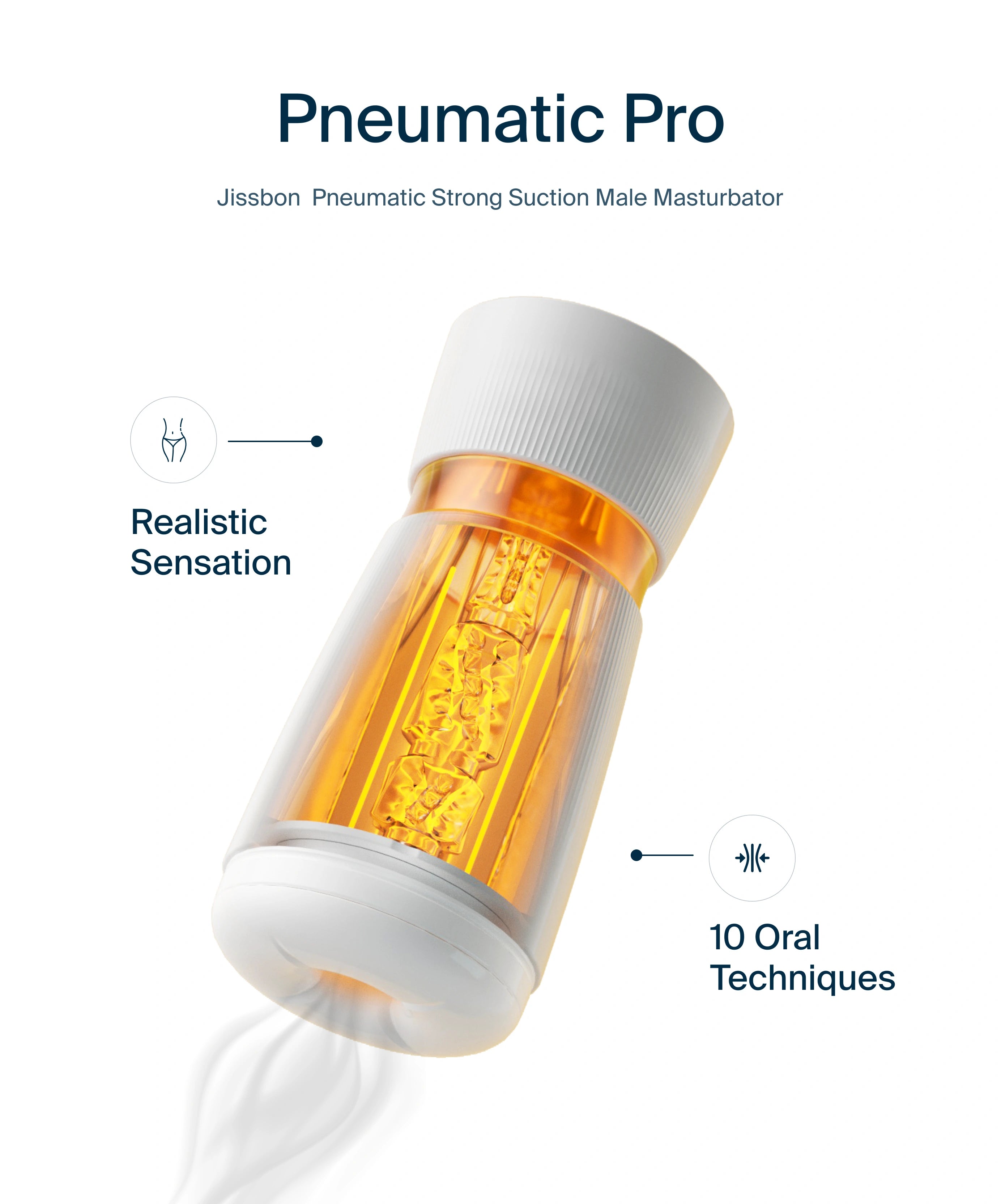
Try this a soft clitoral suction toy or a low‑intensity bullet for 5–10 minutes, 3–4 days a week, as “circulation training.” Start low and stop if you feel sore. Explore discreet options in our Clitoral Vibrators or a gentle, beginner‑friendly model like the Clitoral Suction Vibrator.
Treat clitoral hood adhesions early
If the glans seems “buried” or retracts painfully, ask about clitoral hood adhesions/phimosis. Dermatology and gynecology societies recommend ultra‑potent topical steroids (often clobetasol) for LS, with procedural release only when necessary. Avoid DIY separation—see a specialist.
Be cautious with “vaginal rejuvenation” lasers
Despite heavy marketing, regulators have warned that energy‑based “rejuvenation” procedures lack approval for treating GSM and can cause burns and scarring. Consider proven options first.
A gentle at‑home routine to support recovery
Goal: Keep tissues comfortable, encourage blood flow, and reduce friction while you and your clinician address underlying causes.
- Moisturize: Apply a vaginal moisturizer 3–5 nights/week. Add a fragrance‑free emollient externally for comfort.
- Warmth & touch: Warm compress over underwear for 5 minutes, then light external touch (no pressing on sore spots).
- Low‑intensity vibration: 3–10 minutes around the clitoral hood/outer labia; pause if you feel numb or sore.
- Lubricate liberally for any sexual activity.
- Lifestyle boosters: manage blood sugar, quit smoking, and consider pelvic floor PT if muscles feel tense or sex is painful.
When to see a clinician (please don’t wait on these)
- New pain, bleeding, or tearing with light touch
- White, shiny, or scar‑like patches, intense itching, or skin cracking (possible lichen sclerosus)
- You suspect adhesions (a “sealed” hood or labial fusion)
- Recurrent UTIs, burning urination, or persistent dryness despite moisturizers (possible GSM needing Rx therapy)
A pelvic exam is usually enough to diagnose GSM and LS; your clinician may check pH, rule out infection, or—rarely—do a small biopsy for skin conditions.
Myths vs. facts
-
Myth: Vibrators “damage” the clitoris.
Fact: Overly intense use can cause temporary numbness, but there’s no evidence of permanent damage from typical use. Many experts now include vibrators in sexual‑wellness care plans. -
Myth: If you don’t have sex, your clit disappears.
Fact: Lack of arousal can contribute to dryness and less responsive tissue, but your clitoris doesn’t vanish. Gentle, regular stimulation can help restore responsiveness. -
Myth: Lasers “fix” atrophy for everyone.
Fact: FDA and professional groups have warned about risks and insufficient evidence for energy‑based “rejuvenation.” Consider guideline‑supported options first.
Safe product picks (discreet & beginner‑friendly)
- Quiet bullets/suction toys for soft, external stimulation—great for re‑introducing sensation without friction. Try a petite option from our Clitoral Vibrators.
- Prefer warm‑up first? Pair with a water‑based lubricant and take your time. If you like a gentle suction feel, explore the compact Clitoral Suction Vibrator.
- You can always start on the lowest intensity and increase slowly. (If anything burns or stings, stop and add moisturizer or talk to a clinician.)
Evidence‑based treatments at a glance
- Lubricants & moisturizers: First‑line comfort care; consider hyaluronic‑acid products if you prefer non‑hormonal.
- Low‑dose vaginal estrogen: Strong guideline support for GSM—improves dryness and tissue health; minimal systemic absorption for most formulations.
- Vaginal DHEA or oral ospemifene: Alternatives backed by major guidelines.
- Treat LS early: High‑potency topical steroids; specialist follow‑up.
- Adhesion management: Estrogen or steroid therapy first; procedural release only when needed.
- Lifestyle: Aim for regular arousal, stop smoking, manage diabetes, consider pelvic floor PT if tightness or pain persists.
Trusted resources & further reading
- Clitoral anatomy & function: Cleveland Clinic overview of the clitoris.
- GSM treatment guidelines: North American Menopause Society position statement (vaginal estrogen, DHEA, ospemifene).
- U.S. professional guidance: AUA/SUFU/AUGS guideline synopsis on GSM, including UTI reduction with low‑dose vaginal estrogen.
- Lichen sclerosus (vulvar skin condition): DermNet NZ and Mayo Clinic (treatment typically high‑potency steroids).
- Postpartum & lactation‑related dryness: AAFP review & clinical trials on postpartum estrogen use.
- Vibrator benefits: ISSM sexual health Q&A and peer‑reviewed review on genital vibration.
- FDA warning on “vaginal rejuvenation” lasers: Safety communications summarized by professional societies.
A supportive closing note
If you’ve typed “can your clit fall off” or “I can’t find my clit,” you’re not alone—and you’re not broken. What you’re noticing is usually reversible with the right combination of lubrication, gentle stimulation, and (when appropriate) clinician‑guided therapy for GSM or skin conditions like lichen sclerosus. Your pleasure matters.
When you’re ready to reintroduce sensation comfortably, explore discreet, low‑intensity options in our Clitoral Vibrators—a small, quiet toy can be a kind, confidence‑building first step. For a curated, gentle option, try the Clitoral Suction Vibrator.
Frequently asked questions
Can your clit fall off?
No. The clitoris is a large, internal erectile organ anchored under the pubic bone; it does not detach. If the glans looks smaller or is hard to find, think hidden glans, adhesions, or atrophy, not “falling off.” See a clinician if you notice skin changes, pain, or bleeding.
What are clitoral atrophy symptoms?
Lower sensitivity, smaller‑appearing glans, dryness or stinging with touch, pain with sex, and sometimes urinary issues if GSM is present. White shiny patches or intense itch point more to lichen sclerosus—get evaluated promptly.
Can clitoral atrophy be reversed?
Often, yes. Local estrogen/DHEA or ospemifene, plus moisturizers, lubricants, and gentle arousal strategies (including vibrators) can make a big difference. Treat LS or adhesions early with specialist care.
I can’t find my clit—what’s happening?
It might be hood adhesions (clitoral phimosis) or tissue thinning from low estrogen. Do not attempt DIY separation. A clinician can assess and treat with topical steroids/estrogen or, rarely, a minor procedure.
Can vibrators cause atrophy or permanent numbness?
No evidence suggests that typical vibrator use causes atrophy. Temporary numbness can happen with very intense, prolonged use—dial it down, take breaks, and choose softer toys. Vibrators are often beneficial for arousal and blood flow.
Read more

Vibrators are meant to bring bliss—not broadcast it. If you’re wondering how to make a vibrator quiet, the good news is there are fast fixes you can try tonight and smarter shopping choices for the...

If you’re shopping your first toy (or upgrading an old favorite), you’ve probably asked: what’s the difference between a dildo and a vibrator? In simple terms, a dildo is typically a non‑motorized ...